Susan A. Stallings-Sahler and Gilbert M. Foley, with consultation and contributions from Marie E. Anzalone
Abstract
Editor’s note: This article is adapted from Linking Sensory Integration and Mental Health: Nurturing Self-Regulation in Infants and Young Children—A thoroughly revised and updated version of Sensory Integration and Self-Regulation in Infants and Toddlers (ZERO TO THREE, 2022). This book was written for a broad multidisciplinary audience of service providers, researchers, and policymakers serving infants, young children, and their families. This edition has been expanded to highlight the intersection of sensory processing, sensory processing disorders, and infant and early childhood mental health (IECMH). Parents and family members may also find the contents helpful in understanding and caring for their child with sensory, self-regulatory, and social–emotional challenges in ways that will also enhance their relationships and family life. Now available at www.zerotothree.org/bookstore.
Individual differences in sensory processing do not inevitably lead to difficulties in development, learning, or social–emotional relationships. However, many more important evidential studies are coming into the literature almost monthly, and it is important to stay informed of their findings on developmental and mental health outcomes of infants and children with different types of sensory processing disorders (SPDs), especially when there is still some confusion around comorbidity with other disorders that appear similar on the surface. This is essential to remember when considering screening and assessment for sensory processing and integration. Greater understanding of these issues along with their impact on self-regulation can equip parents, caregivers, and clinicians to help infants and young children interact more successfully with their social and physical worlds. When children are having difficulty with regulating their arousal, attention, and emotions, the process of screening, assessment, and appropriate referral for sensory and motor processing can lead to meaningful intervention for the child, greater understanding for parents and family, and better coping for everyone.
Both assessment and intervention for SPDs need to capture the complexity and interactive nature of development across domains and in relational context. Thus, assessment of young children needs to be both systematic and multidimensional reflecting a general shift in perspective toward integration. Regulatory and sensory processing capacities need to be understood in the context of social–emotional development, relational patterns and disorders, historical contributions, health and well-being, and psychosocial stressors and protective factors (Speranza et al., 2018; ZERO TO THREE, 2016). In this chapter/article, the authors focus on the identification of sensory processing and sensory based-movement disorders, illuminated by the principles and practices of infant and early childhood mental health which will be highlighted throughout.
The Steps of Screening and Assessment for SPDs
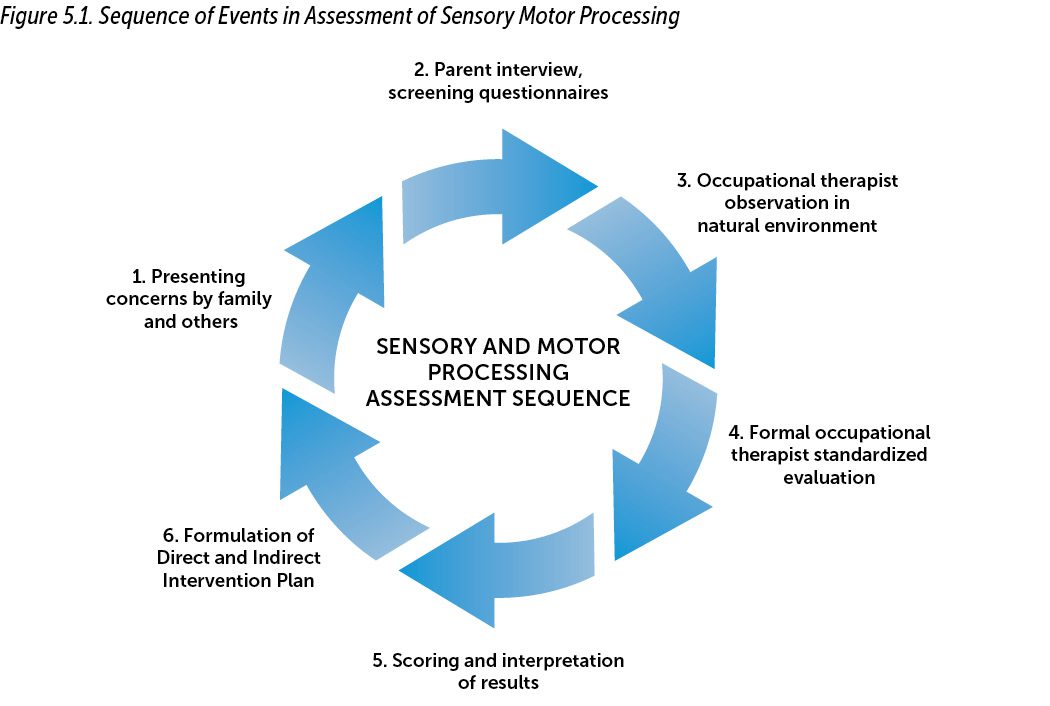
In this chapter, we present general guidelines for screening and assessment of children’s sensory and movement processing within natural environmental contexts.... Figure 5.1 diagrams the process of screening and assessment of sensory and
motor processing.
This set of procedures (see Figure 5.1) is initially triggered by functional and behavioral concerns observed by people in the child’s various social environments, including his own proximal regulatory environment—home, family, school (teachers and peers), and community—that cannot be explained simply as “developmental delay.” These concerns as well as the use of brief screening tools, such as the Short Sensory Profile (McIntosh et al., 1999), provide initial screening data, which may be utilized by mental health or early intervention professionals to make a referral decision for further in-depth evaluation by an occupational therapist. Assuming this occurs, the occupational therapist may first observe the child informally and then conduct the formal assessment soon after. The occupational therapist scores and interprets the data in the context of information provided by involved caregivers and professionals, including parents, teachers, physicians, and mental health professionals. If involved, an infant and early childhood mental health professional may also contribute data regarding family history, relational patterns, social–emotional development, psychosocial stressors, and health contributions. Most important, the occupational therapist, in collaboration with these professionals, applies this integrated interpretation to explain the presenting concerns that precipitated the referral. This leads not only to development of goals and objectives for occupational therapy intervention (if warranted), but also to recommendations for parents and professionals in the social environments in which the child participates. These recommendations usually include adaptations to the sensory, physical, relational, and procedural environments to support the child’s self-regulation and ability to participate more successfully across contexts, relationships, and developmental domains.
The key to screening and assessment of sensory integration is to focus on how the child responds to sensory information and manages environmental challenges inherent within daily routines and activities such as sleeping, feeding, bathing, dressing, exploration, play, and preacademic activities—any of which may involve social interaction. Because sensory integration is about the process through which an infant or child organizes sensory input for functional use, tests or developmental schedules that simply measure whether a child can demonstrate mastery of specific skills will not inform clinicians whether a child might benefit from sensory-based intervention by an occupational therapist. Instead, assessment involves systematic observation of the child, the physical environment, the social environments within which the child moves and interacts, and the dynamic goodness-of-fit among them.... Thoughtful observation of the child is required to try to ascertain not only the “what” of the child’s performance, but the “how” (e.g., how she behaves in the situation) and to explain the “why” if sensory modulation or movement/praxis issues are impairing self-regulation, adaptive functioning, and social relationships. Parent perceptions, attributions of cause and meaning, and quality of interactional and caregiving patterns, objective and subjective, are carefully considered in any formulation.
For instance, Ms. Thompson, a preschool teacher, noted that one of her students, Mario, was unable to participate in classroom coloring and fine motor activities (the “what”) because he was constantly covering his ears with his hands (the “how”). She requested a classroom screening from an occupational therapist. Together they observed Mario and concluded that he might have auditory hypersensitivity to the ambient classroom noise (the “why”), which was worsened by the noise of chair legs scraping against the floor. The occupational therapist provided soft earplugs to the student, which Mario tolerated well. He immediately stopped covering his ears with his hands and was able to complete table tasks successfully. The following week, the occupational therapist returned with a box of used tennis balls. Together, she and Ms. Thompson prepared and placed them over the bottoms of the chair legs, which lowered the noise level for the entire class. It was also recommended for Mario to receive a more in-depth evaluation of sensory processing and to observe him in other school situations. In contacting the mother for more information and permission to evaluate Mario, his mother voiced concerns about Mario’s seeming tendency to tune out and “ignore” her in their busy, lively, and sometimes noisy home environment. Her concerns were carefully considered, and suggestions were made for creating a quiet corner for Mario to play, as well as creating a special daily sharing time for Mom and Mario in a consistent, contained, calm, and quiet space. Attention was paid to reframing Mario’s perceived ignoring and rejection of Mom as having a sensory and not an emotional/attachment meaning.
As this scenario demonstrates, goodness-of-fit can refer not only to the child within the relational context of the family, but also between the child and her environment with all of its demands on sensory processing and self-regulation. The value of qualitatively assessing the infant or child, the activity, and the surrounding environment to determine why the “fit” is not working is evident. It should be noted that the environmental and home adaptations (earplugs and dedicated space suggestions) addressed that situation for that particular child; however, in the greater scheme of his needs, it did not address the impairment of his personal auditory oversensitivity, which was hampering his function in other settings as well. Furthermore, children seldom have just one isolated sensory processing issue—it may simply be the most obvious one, so it is advisable to look beyond the “tip of the iceberg.” Experienced therapists trained in sensory integration evaluation know that there tend to be patterns of high and low scores that cluster together and know what to look for.
Guidelines for Screening and Assessment of Sensory Processing,/h2>
A screening provides an overall measure of the child’s functioning in a particular domain and identifies whether there is a need for further assessment. A professional who is knowledgeable about child development from any of a variety of disciplinary perspectives can conduct a screening that may point to the possibility of an SPD. However, evaluation of a child’s functioning in each area of concern should be conducted by a professional with specialized training in that domain. Thus, a well-trained primary health care provider, early caregiver, early intervention provider, or mental health practitioner could screen a child to determine whether he is having problems in sensory modulation or general motor control. However, an occupational therapist would be the most appropriate professional to complete a comprehensive assessment of sensory integration.
The following guidelines establish important parameters for performing quality screening and assessment of sensory integration:
1. Focus on how the child responds to sensory characteristics of the environment and objects in it as well
as how she manages adaptive challenges. This area of function is not about specific skills or milestones achieved. Rather, it entails a dynamic process orientation to assessment in addition to the end-product focus typical of most developmental evaluations (Rahlin et al., 2019). For example, let’s say the clinician is interested in whether a child has achieved the developmental milestone of being able to build a seven-block tower. However, it is noted that from a process perspective, clinicians are also interested in analyzing qualitative aspects of the infant or child’s performance, such as bilateral hand use, hand/finger grasp patterns, efficiency of construction, accuracy of block edges, attention, task persistence, frustration tolerance (if the tower falls); whether performance varies in different contexts, relationships, affective states and so forth. If an evaluator observes a child engaging in repetitive rocking, he should ask whether this occurs within all environments and relationships, as well as what conditions tend to precede or follow these episodes.

Goodness-of-fit can refer not only to the child within the relational context of the family, but also between the child and her environment with all of its demands on sensory processing and self-regulation.
2.Utilize parent interview, and have them complete questionnaire(s) that provide additional screening and assessment data about the child in natural, familiar settings. These should be primary methods of gathering information about a child’s capacity to process sensory input within the contexts of family relationships, play, and functional activities (occupational therapists call them “occupations”). This approach to interviewing incorporating a style of “tell me about a typical day” is discussed later. It is especially helpful to speak with caregivers about their experiences, objective and subjective, but also to observe the child directly in situations such as
the following:
• mealtimes at home and other places such as child care or out in a restaurant (if this is identified as a problematic setting);
• bathing, toileting, toothbrushing, and hair/nail care;
• independent play and free play with peers;
• parent–family interactions and differing relationships and affective states (e.g., separation anxiety); and
• transitioning between environments and activities.
If the family member appears reticent about completing forms, the clinician should offer to discuss the questionnaire in the format of an interview. Often parents are not sure how to interpret questions about the sensory processing behaviors being asked on the forms or the Likert-type response scales provided. Regardless of the method used, it is always wise for the evaluator to review the responses and to get clarification and examples from the informant to ensure accuracy of reporting.
3. Examine the “fit” between the child and his environment. If logistically possible, we should never look at a young child in isolation or outside the context of their primary caregiving relationship during the assessment process; in addition, we should always identify strengths as well as possible signs of a problem. Reflect on the fact that functional issues can arise from a poor fit between the child’s sensory or motor needs, resources for self-regulation, and demands of the surrounding relational and/or physical environments. For instance, if a child seems distractible during play or the evaluation session, we should “tune in” to the surroundings and ask ourselves whether there is something in the environment that is pulling the child’s attention away, intensifying or muting an affective state, or raising her state of arousal such as the lighting or busy sounds and activities in the playroom. (Often the examiner has habituated to the same stimuli that are distracting the child.) Is she sitting on a surface that is so high that her feet can’t touch the floor or footrest? If appropriate for the setting, is her caregiver nearby? Does the child’s performance improve if we make adjustments to the sensory environment by adapting her seating to provide better support, or by being sure her caregiver is in eye-shot? Recall Als’s (1986) synactive model and how a stressed postural–motor system can lead to deterioration of the attentional system. Occupational therapy practitioners often use the metaphor of a nutritional diet composed of various nutrients needed to maintain health to describe the idea of the composition of a person’s daily exposure to sensations that support health and function of the brain and nervous system. Sometimes simple changes to the child’s ongoing “sensory diet” can bring about significant enhancement in her functional responses—another aspect to
dynamic assessment.
4. Sensory input can build up over time before it is responded to. We must keep in mind that the phenomenon of summation can occur over the course of an hour or a day as well as during treatment sessions. A young child who is sensitive to sound may be able to “hold it together” all day at school; however, by the time he is picked up after school, the last thing he may want is to “talk about his day” or to sit at a table and have therapy or assessment task demands made on him. Another child may be slow to register input because of a high threshold but may rapidly become overloaded by accumulated sensation. The evaluator must take care to make changes to the type and amount of sensory input provided to the child during evaluation in a gradual, understated manner. Sometimes offering a brief “bio break” for water, bathroom, or just to touch base with the parent can provide a “reset” that helps the child to continue with assessment activities.
5. Notice and keep track of the child’s arousal level throughout the assessment because it influences sensitivity to the environment. If the child is highly aroused (physiologically and emotionally), it is more likely she will respond to surroundings in a hyper-responsive or disorganized way. A child coming for evaluation immediately after a holiday party can be expected to need some “cool down” time. However, a child who is under-aroused will tend to respond more sluggishly and appear hyposensitive to input. Therefore, we should first determine from an adult familiar with the child whether this level of arousal is typical for her, and if so, it should be used as a baseline for interpreting behavior and responses. Any extremes will bias our findings and interpretation. With this in mind, it is important not to base all of our conclusions about the child’s sensory processing functions on one observation session. It is expected that the behavior of young children will be inconsistent. Babies and toddlers are generally more variable from day to day—children with SPDs even more so. Therefore, the clinician must always consider if the sample of behavior is representative and reliable. At any given time, the consistency of a child’s behavior can be influenced by (a) the type and degree of stimulation in the surroundings, (b) the child’s current emotional state and coping skills, (c) the accumulated sensory “build up” (especially in the afternoon), and (d) the availability of a familiar caregiver in the setting.
6. Include some evaluation procedures that provide opportunities for free play, but include observation with evaluator-chosen toys that bring out self-initiation, creativity, and flexible problem solving during the assessment process. If possible in the setting, it is also helpful to observe the caregiver in play with her child, teaching a task, setting a limit, and meeting a need. Try not to over-structure the free-play assessment environment, but use developmentally appropriate toys and small play equipment (e.g., soft tunnel, scooter board, small ball pit) that invite exploration, interaction, and movement. Examiner and parents need to step back for a period of time and avoid pressing the child to do things a certain way. Rather, see what draws his interest versus what he tends to avoid. Directiveness by the examiner, although necessary for certain styles of testing, can restrict expression of individual differences or precipitate excessive performance anxiety during qualitative observation. This unstructured time is also valuable for observing praxis (a child’s ability to conceptualize, organize, and implement unfamiliar actions) as well as postural tone, dynamic position transitions during play, and spontaneous bilateral movements. After observing what the child can do spontaneously, the examiner should note areas of potential difficulty and then present a “doing model,” providing the child an opportunity to imitate the action(s). A stuffed animal going through the soft tunnel, or riding on the scooter board or platform swing, may be enough to provide the ideational “suggestion.” It is also important not to overwhelm a young child with verbal directions of “what to do” and be mindful of the child’s level of comprehension and verbal processing capacities. See whether he can get the idea using the visual cues and by mapping his own somatosensory body scheme to the affordances of the objects. Simple narrative verbal cues—such as “beep-beep” or “Here goes teddy through the tunnel!” or heightening, modulating, or muting your affect —may add interest and an action suggestion without being directive.
It is important not to base all of our conclusions about the child’s sensory processing functions on one observation session.
Observation of the Child: What to Look For
It is not within the scope of this book to provide exhaustive detail for assessing all areas of sensory processing/integration and praxis. There are several standardized screenings, parent–teacher questionnaires, and performance-based tools, although not all are appropriate for the population of birth to 3 years old (a few more can be used with 4- and 5-year-olds). Short screenings and parent–teacher questionnaires may be used by non–occupational therapy professionals as means for preliminary identification. Preferably, all assessment occurs within a relationship between child, family, and assessor, conducted as a supportive process.

Skilled observation focuses on the influence of sensory input on the child’s self-regulation of levels of arousal and attention, posture and movement organization, as well as socioemotional behaviors.
If dysfunction is suggested, results should be validated by a more performance-based evaluation from an occupational therapist with appropriate training in sensory integration assessment, and an intervention plan for interdisciplinary application should be developed. Current screening and questionnaire-based tools include the following:
• Short Sensory Profile (McIntosh et al., 1999),
• Sensory Profile 2 (Dunn, 2014),
• Sensory Processing Measure: School Form (Parham et al., 2007), and
• Sensory Processing Measure: Home Form (Miller-Kuhaneck et al., 2007).
Skilled observation focuses on the influence of sensory input on the child’s self-regulation of levels of arousal and attention, posture and movement organization, as well as socioemotional behaviors. Before arranging an assessment session, it is helpful to find out from the parents “when and where” the child would feel the most comfortable and affectively available to participate in the assessment process. It may be that an evaluation split into two sessions will provide the best scenario, depending on the child’s age, the concerns, and various logistical factors such as travel required for family (if any). Although observing the child in her natural environment is an important aspect of any assessment, it is generally difficult to conduct many standardized evaluations in the home because we are on the child’s “turf,” and she may feel less inclined to respond to boundaries imposed by the evaluation itself, such as sitting at a table next to the examiner or following directions while moving about on the floor.
The following assessment and observational points are arranged generally in developmental order, starting as follows: (a) sensory modulation (i.e., sensory over-responsivity/sensitivity, sensory under-responsivity, and sensory seeking/craving), (b) postural and bilateral integration (e.g., when age appropriate, observations of postural tone, righting responses, position transitions, ocular fixation and pursuits, bilateral body movements, midline movements, and side preference), and (c) praxis (of different types, such as whole-body imitation, ideation, verbally mediated actions, or manipulating objects). It is essential to understand that these are examples of responses that may be elicited. In assessment, we look for patterns or clusters of several behaviors together. A child need not show all of the symptoms; conversely, just having one or two may simply suggest normal individual differences that do not interfere with function or relationships. However, it is always better to screen and refer the child with a possible sensory developmental atypicality—which, after further evaluation, turns out to be a false positive—than it is to conclude there’s “nothing to see here,” when in reality that conclusion is a false negative, and the referral ball is dropped, denying the child further evaluative benefit and possible intervention (Glascoe, 2001).
Bear in mind that these observations need to be corroborated as much as possible using professional standardized measures. Nonetheless, they serve as valuable guideposts that point the way toward meaningful assessment and intervention and all assessment data must be understood through the lens of relationships, affect, culture, community, and family values.
Learn More
Linking Sensory Integration and Mental Health: Nurturing Self-Regulation in Infants and Young Children
Susan A. Stallings-Sahler and Gilbert M. Foley, with consultation and contributions from Marie E. Anzalone www.zerotothree.org/bookstore
Author Bios
Susan A. Stallings-Sahler, PhD, OTR, FAOTA, is an occupational therapist, educational psychologist, and director of Developmental Research and Education Consultants, LLC, in the Tampa Bay area. During the writing of this book, she served as professor and doctoral project coordinator at Gannon University’s (FL) Occupational Therapy Doctorate program. Dr. Stallings-Sahler has more than 40 years of clinical, academic teaching, research, and leadership experience in pediatric rehabilitation—including neonatal intensive care unit and early intervention. Dr. Stallings-Sahler completed an advanced postgraduate internship at USC’s Ayres Clinic, studying with A. Jean Ayres, founder of the sensory integration theory and approach. Dr. Stallings-Sahler is the author of the Screening Assessment of Sensory Integration (SASI), and has published more than 40 scholarly articles and chapters.
Gilbert M. Foley, EdD, IMH-E, serves as consulting clinical psychologist at the New York Center for Child Development in New York City and clinical co-director of the New York City Early Childhood Mental Health Training and Technical Assistance Center. He is endorsed as an infant mental health/ clinical mentor, Level IV, and is a founding board member of the New York and Pennsylvania State Associations of Infant Mental Health. He is a senior faculty member of the DIR® Profectum Academy and is on the editorial board of the Journal of Infant, Child, and Adolescent Psychotherapy. Dr. Foley is the coauthor of three books and has written more than 40 scholarly articles and chapters.
Marie E. Anzalone, ScD, OTR, FAOTA (1952–2021). During the early phase of planning this manuscript, Dr. Anzalone was an occupational therapist in private practice in San Diego where her practice, Kid Power OT, served children from birth to 3 years old through Early Start. She was previously a professor of occupational therapy at Columbia, Virginia Commonwealth, Duquesne, and Boston universities. She was recognized as a fellow by ZERO TO THREE as well as by the American Occupational Therapy Association for her work with infants and families. As a Fulbright Scholar at the University College in Cork, Ireland, she worked to bring infant mental health, clinical reasoning, and the study of play to the forefront of practice with infants.
Suggested Citation
Stallings-Sahler, S. A., & Foley, G. I. (with Anzalone, M. E.). (2022). Identification of sensory processing and sensory-based movement disorders in infants and young children. ZERO TO THREE Journal, 43(1), 39–45.
References
Als, H. (1986). A synactive model of neonatal behavioral organization: Framework for the assessment of neurobehavioral development in the premature infant and for support of infants and parents in the neonatal intensive care environment. Physical and Occupational Therapy in Pediatrics, 6, 3–53.
Dunn, W. (2014). The Sensory Profile 2. Pearson Assessments.
Glascoe, F. P. (2001). Are over-referrals on developmental screening tests really a problem? Archives of Pediatrics & Adolescent Medicine, 155(1), 54–59.
McIntosh, D. N., Miller, L. J., Shyu, V., & Dunn, W. (1999). Overview of the Short Sensory Profile. In W. Dunn (Ed.), The Sensory Profile: Examiner’s manual (pp. 59–73). Psychological Corporation.
Miller-Kuhanek, H., Henry, D., & Glennon, T. (2007). Sensory Processing Measure: School Form. Western Psychological Services.
Parham, L. D., Ecker, C., Miller Kuhaneck, H., Henry, D. A., & Glennon, T. J. (2007). Sensory Processing Measure. Western Psychological Services.
Rahlin, M., Barnett, J., Becker, E., & Fregosi, C. M. (2019). Development through the lens of a perception–action–cognition connection: Recognizing the need for a paradigm shift in clinical reasoning. Physical Therapy, 99(6), 748–760.
Speranza, A. M., Malberg, N., & Steele. M. (2018). Mental health and developmental disorders in infancy and early childhood: The PMD-2. Psychoanalytic Psychology, 35(3), 328–338.
ZERO TO THREE. (2016). DC:0–5TM: Diagnostic classification of mental health and developmental disorders of infancy and early childhood.




