
Supporting States in Building a Robust Continuum of Mental Health Systems and Services for Infants, Young Children, and Families


Key Takeaways
- In the first five years of life, children develop more rapidly than at any other time in the lifespan.
- During this period, relationships are at the heart of everything. The health and well-being of babies and young children are rooted in early relationships that are nurturing, responsive and supportive, and are nested in their community, culture and language.
- Babies and young children can experience mental health conditions caused by trauma, neglect, and biological or environmental factors.
- Health and healing can be promoted through developmentally specific, culturally resonant approaches that support families and address mental health conditions.
- Historically, the health care infrastructure has not prioritized the mental health needs of infants and young children. However, states nationwide are working to increase access to the full continuum—promotion, prevention, developmentally appropriate assessment and diagnosis, and treatment—of high-quality mental health supports and services for young children and their caregivers.
The Infant and Early Childhood Mental Health (IECMH) Financing Policy Project (FPP)
ZERO TO THREE recognized that a collective learning approach—bringing states together for mutual problem-solving—might be more effective and efficient than traditional one-on-one technical assistance models.
We launched the Infant and Early Childhood Mental Health (IECMH) Financing Policy Project (FPP) in 2016. Since then, it has served as a learning collaborative for 36 states. Colleagues in states and communities sought guidance on how to build IECMH systems, particularly those supporting assessment, diagnosis and treatment.
With support from the Irving Harris Foundation, Klingenstein Philanthropies, W.K. Kellogg Foundation, Robert Wood Johnson Foundation, Perigee Fund, Alliance for Early Success, an anonymous donor and the University of Minnesota, ZERO TO THREE implemented a relationship-based strategy to advance state IECMH policy.
This strategy included three components:
- An online learning community
- Peer-to-peer and expert technical assistance to address specific issues
- In-person convenings of multidisciplinary state teams with the capacity and authority to implement policy changes
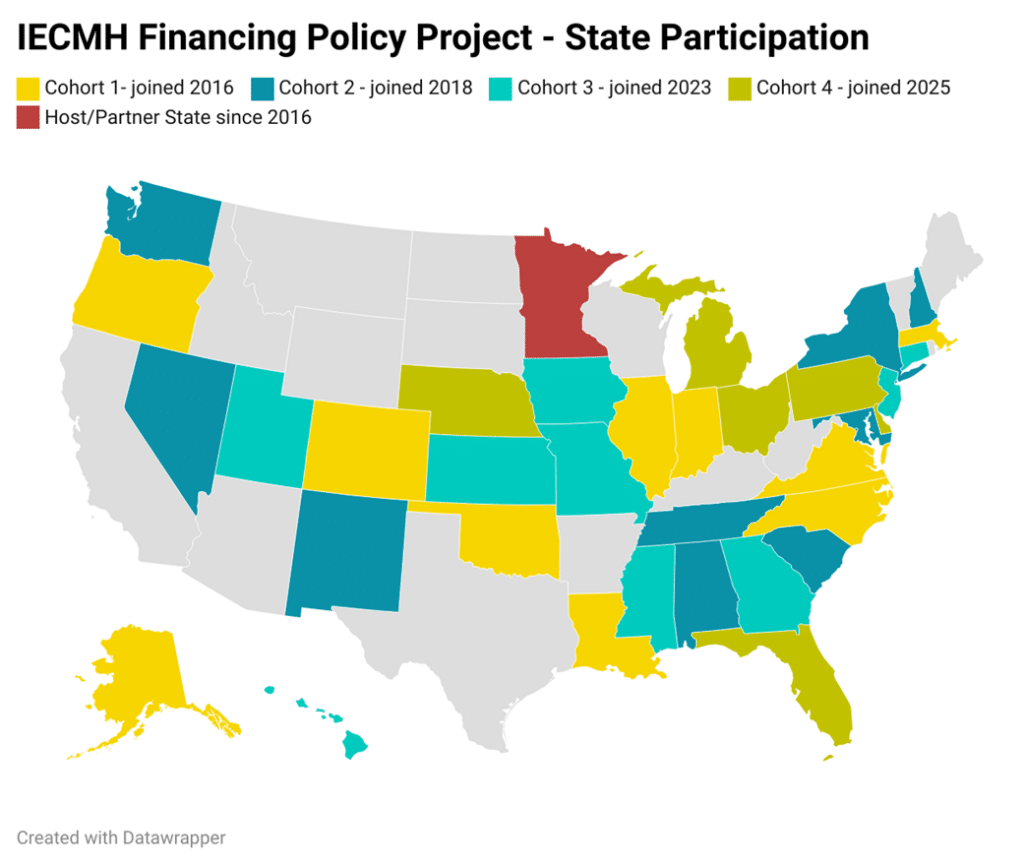
In October 2016, the first cohort of 10 states convened to focus on improving assessment, diagnosis and treatment. Participating teams included Alaska, Colorado, Illinois, Indiana, Louisiana, Massachusetts, North Carolina, Oklahoma, Oregon and Virginia, along with expert contributors from Minnesota.
Subsequent cohorts were selected as follows:
- 2018: Alabama, District of Columbia, Maryland, Nevada, New Hampshire, New Mexico, New York, South Carolina, Tennessee and Washington
- 2022: Connecticut, Georgia, Hawaii, Iowa, Kansas, Mississippi, Missouri, New Jersey and Utah
- 2024: Delaware, Florida, Michigan, Nebraska, Ohio and Pennsylvania
All four cohorts came together March 17–19, 2025, in Minneapolis for a national convening. The gathering offered a valuable opportunity for state teams to connect, share experiences, surface challenges and learn from one another and national leaders.
It was a wonderful convening in Minneapolis, and I hope they can continue! I always learn so much, and there is no other conference or space that has the information and knowledge that I gain from the FPP overall and the networking with so many states in the same room together."
Convening Participant

State Accomplishments
States from Cohorts 1, 2 and 3 made meaningful progress during their technical assistance cycles.
Highlights include:
Hawaii strengthened relationships with leaders in the Department of Health and Medicaid. The state is adopting DC:0–5™ Diagnostic Classification of Mental Health and Developmental Disorders of Infancy and Early Childhood and developing a crosswalk through a workgroup of IECMH clinicians, Med-QUEST clinicians and a health plan coding expert.
The FPP team is also designing a bundled payment pilot that would allow clinicians to receive a single payment for a defined set of IECMH services each month. This streamlined billing process allows best practice services to be provided and paid for, including extended assessment before requiring a diagnosis, care coordination, dyadic and family-centered treatment, and home- and community-based treatments. A provider survey was distributed to understand service delivery gaps, training needs, geography and billing issues.
Utah collaborated with the Children’s Funding Project to adapt its fiscal map tool with a focus on IECMH. The team is developing a finance map to clarify existing funding streams and worked closely with the state Medicaid director to understand billing for IECMH services.
This collaboration clarified that several billing pathways already existed. As a result, Utah’s action plan shifted from policy development to maximizing current pathways. Administrative changes also improved the EPSDT approval process, reducing pre-approval time from two weeks to just three days.
Kansas created a three-year implementation plan for DC:0-5, requiring provider training and use for Medicaid billing. The plan includes multi-session assessments with at least five sessions before diagnosis and treatment. Kansas also:
- Expanded services beyond community mental health centers
- Added Parent Peer services to Medicaid
- Developed an “IECMH System Flow” diagram to guide pediatric providers
- Engaged in autism planning and funding stream mapping
With funding from the DC Council, the Department of Health Care Finance led a citywide Perinatal Mental Health Task Force and released a comprehensive report. The city increased IECMH consultation funding by $15 million over several years and expanded HealthySteps access, resulting in a 500% increase in families served over three years.
DC is also developing an infant mental health framework for early intervention to build capacity among interventionists.
Massachusetts created an IECMH strategic plan and established two key positions: one in state government and one via a public-private partnership with MassAIMH and the Massachusetts Society for the Prevention of Cruelty to Children (MSPCC). The state invested in infrastructure, reflective consultation opportunities and a statewide web-based reflection series.
Massachusetts also emphasized DC:0-5 training. Nine trainers have trained more than 700 practitioners, pairing training with reflective case consultation for effective learning.
The FPP is like having 150 mentors. We now have research, practice, and policy connections."
Project Participant

The Impact of the FPP
Over eight years, the FPP has become a powerful mechanism for advancing IECMH systems and policy across the country. Its collective learning model has led to significant innovations.
- Thirty-six states are actively pursuing IECMH policy
changes. - Thirty-five states attended the 2025 convening.
- More than 23 states have requested ongoing technical assistance, the highest engagement in the program’s history.
FPP state teams have:
- Drafted policy language requiring or allowing use of DC:0-5 to improve assessment and diagnosis.
- Created crosswalks between DC:0-5 and DSM/ICD (Diagnostic and Statistical Manual/International Classification of Diseases) codes for eligibility and billing.
- Drafted and implemented federal and state Medicaid policies that support IECMH.
- Trained hundreds of professionals in DC:0-5 and evidence-based treatment strategies.
- Developed innovative, state-specific IECMH system strategies tailored to state priorities.
- Identified new and diversified funding and sustainability mechanisms, including Medicaid, to support IECMH services and systems.
- Created dedicated IECMH positions in state government
- Established or strengthened IECMH professional associations.
- Cultivated influential champions for IECMH within states.
The FPP has created a strong root system to infuse IECMH. When the sun is shining, we can grow, when stormy, we can stay and have community, technical assistance, and plan."
Project Participant
