Laura M. River, Angela J. Narayan, and Thania Galvan, University of Denver
Luisa Rivera, Emory University
William W. Harris, Children's Research and Education Institute, New York, New York
Alicia F. Lieberman, University of California, San Francisco
Abstract
During pregnancy, low-income women are at high risk for depression and posttraumatic stress disorder (PTSD), but they are unlikely to receive mental health services. As a follow-up to Narayan et al. (2017), we provide a detailed picture of pregnant women’s mental health service (MHS) need versus utilization. Results suggested that the majority of women with very elevated depression and PTSD symptoms received MHSs during pregnancy. However, few women with lower-grade depression received MHSs, despite meeting prenatal depression criteria recommended by the American Academy of Pediatrics. Pregnant women of color were also especially unlikely to receive MHSs. Inefficient transportation and lack of child care were primary issues interfering with service utilization. Detailed recommendations for how to improve MHS access are discussed.
Pregnancy is often heralded as among the most joyous and exciting times in a woman’s life. Less often discussed, however, are the risks of pregnancy to mothers’ mental health. During pregnancy, women face immense upheaval and change in virtually every domain of their lives—including romantic and family relationships, personal identity, physical health, and finances—and they often confront tremendous uncertainty about all that is ahead (Slade, Cohen, Sadler, & Miller, 2009). This transition can be especially fraught for women with histories of childhood trauma, who often struggle with distressing reminders of their own difficult upbringings and concerns about their ability to parent differently than they were parented (Lieberman, Diaz, & Van Horn, 2009; Narayan et al., 2017). For some pregnant women, these stressors may contribute to the onset or exacerbation of mental health problems.
Indeed, there are markedly higher rates of psychological disorders commonly associated with childhood trauma, particularly depression and posttraumatic stress disorder (PTSD), during pregnancy (Choi & Sikkema, 2016; Narayan, Rivera, Bernstein, Harris, & Lieberman, 2018; Seng et al., 2010). In fact, contrary to public perception, rates of prenatal depression are consistently higher than rates of postpartum depression (Underwood, Waldie, D’Souza, Peterson, & Morton, 2016). Risks for depression and PTSD are even greater among low-income and ethnic-minority pregnant women, who tend to report higher levels of childhood trauma and more severe, chronic prenatal stress (Choi & Sikkema, 2016; Lancaster et al., 2010; Seng et al., 2010). In turn, prenatal depression and PTSD can negatively affect maternal well-being and health behaviors, birth outcomes, infant development, and mother–infant relationships (Seng et al., 2013; Vanderkruik, Lemon, River, & Dimidjian, in press; Vesga-López et al., 2008). Clearly, these issues represent a significant public health concern.
Despite the clear and pressing mental health service (MHS) needs among expectant mothers, rates of MHS utilization during pregnancy are generally low (Cook et al., 2010; Kelly, Zatzick, & Anders, 2001). Women are unlikely to receive MHSs, even when they meet clinical thresholds for psychological disorders that are accurately detected by prenatal care providers (Kelly et al., 2001). Notably, pregnant women with mood or anxiety disorders are significantly less likely to receive MHSs than their non-pregnant peers with the same disorders (Vesga-López et al., 2008). Pregnant women are also less likely than postpartum women to receive services for similar mental health problems (Glasheen, Colpe, Hoffman, & Warren, 2015). This phenomenon is even more striking given that, during pregnancy, women may have the most contact with the health care system of any period in their lives. Yet, MHSs do not seem to adequately reach pregnant women, to the detriment of their own—and their babies’—health and well-being.
What is responsible for the stark mismatch between elevated prenatal MHS need and low prenatal MHS utilization? How can MHS providers better serve pregnant women in need of care? This article pursues answers to these questions in a clinical research study of low-income, ethnically diverse pregnant women, with high rates of childhood and lifetime trauma, who were receiving prenatal care at an urban safety-net hospital. In a previous article using the same sample, we identified that women had an alarming level of unmet MHS need during pregnancy (Narayan et al., 2017). In this follow-up, we provide a detailed picture of those women’s prenatal MHS utilization, as reported during pregnancy and at 3–4 months postpartum. We investigate factors that may contribute to the gap between prenatal MHS need and utilization, including sociodemographic characteristics (e.g., poverty status, race/ethnicity) and severity of depression and PTSD symptoms. Finally, we provide recommendations for MHS providers and agencies, informed by participants’ insights into barriers to accessing services and their recommended solutions to improve services.
Method
The study design and sample characteristics are fully described in our previous article in this journal (Narayan et al., 2017). To review briefly, we recruited 101 pregnant women in their second or third trimester who planned to deliver at Zuckerberg San Francisco General Hospital and Trauma Center (ZSFG), a safety-net hospital serving predominantly low-income families. Women were predominantly recruited from prenatal appointments at the ZSFG obstetrics/gynecology clinic, and via fliers posted at the hospital and other community clinics and agencies serving low-income pregnant women. Of 101 women, 70% were living below the federal poverty line. Women were diverse in terms of ethnicity (37% Latina; 22% African American; 20% White; 7% Asian or Pacific Islander; 1% Native American; 13% biracial or multiracial), national origin (37% were foreign-born), and primary language (26% were monolingual Spanish-speaking). They reported high levels of childhood trauma (e.g., maltreatment, domestic violence exposure) on the Adverse Childhood Experiences Scale (ACEs; Centers for Disease Control and Prevention, 2016) and high levels of adulthood stress (e.g., homelessness, intimate partner violence). A substantial proportion (22%) of women were unpartnered with the baby’s father during their pregnancies.
Participants completed two interviews, one during pregnancy and one at 3–4 months postpartum. Interviews were conducted in the participant’s preferred language (English or Spanish). Each interview lasted approximately 2 hours. Interviewers offered women MHS referrals in their preferred language and in a culturally sensitive manner
Measures
Interviews included questions about demographics, mental health, life experiences, relationships, MHS need, and MHS utilization. Participants also gave permission for medical record extraction from their prenatal, labor, and delivery medical records.
Sociodemographic Variables
We examined the following sociodemographic variables related to MHS need and utilization: maternal age, ethnicity (White or non-White), foreign-born status (yes or no), educational attainment (years), monthly income, federal poverty status (yes or no, based on income-to-needs ratio corresponding to U.S. federal poverty guidelines), homelessness during pregnancy (yes or no), gestational age (weeks), first pregnancy (yes or no), relationship status with the baby’s father (partnered or unpartnered during pregnancy), and ACEs reflecting childhood maltreatment (e.g., emotional abuse, physical neglect) versus family dysfunction (e.g., parental mental illness and substance use problems).
MHS Need
We assessed prenatal MHS need with standardized instruments for depression symptoms (Edinburgh Postnatal Depression Scale, EPDS; Cox, Holden, & Sagovsky, 1987) and PTSD symptoms (PTSD Checklist for DSM-5, PCL-5; Weathers et al., 2013), and mental health diagnoses listed on labor and delivery medical records. Pregnant women were categorized as having prenatal MHS need if they reported clinical levels of depression symptoms on the EPDS (scores ≥ 10, the cutoff recommended by the American Academy of Pediatrics, AAP; Earls, 2010), clinical levels of PTSD symptoms on the PCL-5 (scores ≥ 33; National Center for PTSD, 2019), or had a mental health diagnosis listed on their medical charts.
MHS Utilization
We assessed prenatal MHS utilization in three ways. First, during the prenatal interview, we asked women if they were currently attending therapy, counseling, or psychiatry appointments. Second, during the postnatal interview, we asked women if they had attended therapy or counseling at any point during their pregnancy. Third, we reviewed medical records to check if pregnant women were seen in the ZSFG high-risk obstetric clinic for psychiatric services. MHS utilization was coded if any of these three indices were positive.
Barriers and Solutions for MHS Utilization
During the postnatal interview, we asked women about perceived barriers to accessing MHSs and potential solutions to improve access to care. Specifically, we asked: “What makes it difficult to keep appointments?” and “What could mental health agencies or social services do better to care for women?” We conducted thematic analyses of women’s responses to each of these questions. For each question, two coders independently read responses, identified themes, and categorized responses according to those themes. Then, the coders discussed and reached consensus on which themes applied to which responses (a single response could be categorized under multiple themes).

Cultural barriers rather than relative socioeconomic disadvantage may partially explain the gap in mental health service usage based on ethnicity.
Patterns of Prenatal MHS Need and Utilization
On the basis of the criteria described in the previous section, more than two thirds (68%) of 101 women had clinically significant MHS need during pregnancy. This rate of mental illness during pregnancy—with serious implications for maternal and fetal health—is staggering. However, as we predicted on the basis of previous research documenting low levels of MHS utilization during pregnancy, only about half (54%, n = 37) of women with MHS need actually received MHSs at any point during their pregnancies, according to their reports and medical records. This discrepancy between MHS need and utilization echoes previous findings that pregnant women are unlikely to receive MHSs, despite facing elevated risk for psychological disorders, and begs for investigation into barriers to care.
Predictors of MHS Need and Utilization
To unpack the disparity between prenatal MHS need and utilization, we explored whether various sociodemographic or symptom-related profiles contributed to variation in MHS need and utilization.
Sociodemographic Factors
First, we examined whether any sociodemographic variables were associated with MHS need and utilization, using t-tests and chi-square tests. Compared to women without MHS need, women with MHS need were more likely to be living below the federal poverty line (p < .05), be unpartnered with the baby’s father (p < .01), and report greater childhood maltreatment (p < .05). These risk factors are consistent with previous findings that women with childhood trauma and current stress are most vulnerable to prenatal mental illness (Choi & Sikkema, 2016; Lancaster et al., 2010; Seng et al., 2010). Women with MHS need were also marginally less likely to be foreign-born (p < .10) and more likely to report homelessness during this pregnancy (p < .10).

Providers can normalize prenatal mental health problems by explaining that women undergo a tremendous amount of change during pregnancy.
Among those women with MHS need, a few factors differentiated women who received versus did not receive MHSs. Women who had MHS need and received MHSs were more likely to be White (p < .05) and unpartnered with the baby’s father (p < .05), and to report marginally greater childhood family dysfunction (p < .10). Given that being White was a predictor of MHS utilization, but income and poverty status were not, cultural barriers rather than relative socioeconomic disadvantage may partially explain the gap in MHS utilization based on ethnicity. Such cultural barriers could include mismatch between ethnicity of MHS providers and clients, low cultural competence among MHS providers, cultural differences in conceptualization of mental health problems and solutions, and culturally specific stigma surrounding mental health treatment (Brach & Fraserirector, 2000).
We were intrigued by the finding that women who were currently unpartnered with the baby’s father were more likely than partnered women to receive MHSs. Unpartnered women receive less social support than their partnered peers, which may lead them to seek support through MHSs. Unpartnered women may also seek services to cope with the stress of romantic relationship dissolution. Following this logic, pregnant women may be more likely to seek services when there is an identifiable, discrete stressor (e.g., relationship dissolution) to which they can link their symptoms. Alternatively, being in a partnership may discourage women from seeking MHSs for various reasons, such as partners’ attitudes about the legitimacy of prenatal mental health problems. Finally, we were surprised to find that a history of childhood family dysfunction was associated with a marginally greater likelihood of MHS utilization. Given that several of the ACEs family dysfunction items pertain to mental health problems in the family-of-origin (e.g., parental mental illness and substance use), we speculate that women with this family history may be more familiar with mental illness and treatment. For instance, if their own parents received psychiatric treatment and found it helpful, pregnant women might be more inclined to seek out services or accept the recommendation of MHSs by primary care providers.
Symptom Severity
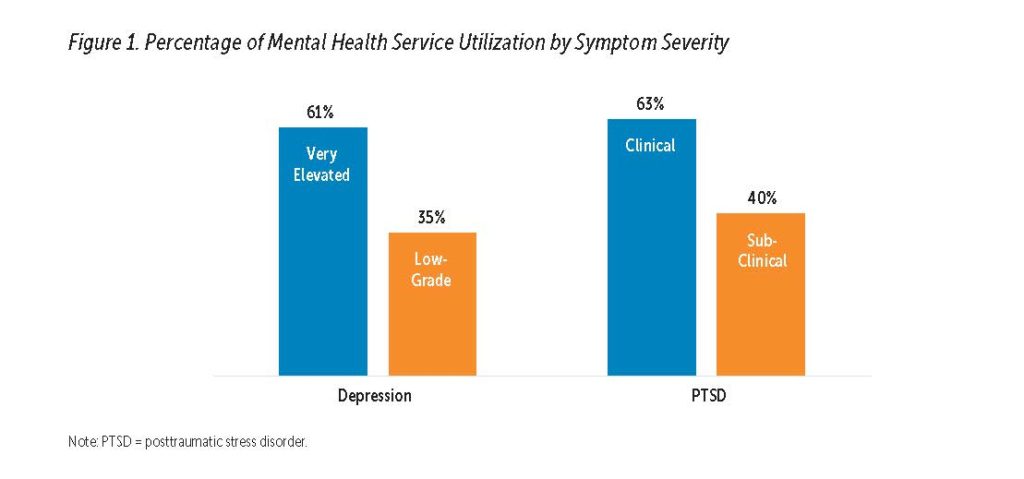
Next, we explored the association between symptom severity and MHS utilization (see Figure 1). For depression, the majority (61%, n = 19) of women with very elevated clinical depression scores—13 and above, the clinical cut-off originally indicated by EPDS developers (Cox et al., 1987)—received MHSs during pregnancy, which is somewhat encouraging. However, only about one third (35%, n = 6) of women with low-grade clinical depression scores (10–12) received MHSs during pregnancy. The AAP recommends an EPDS cut-off of 10 because women with scores of 10–12 are at risk of persistent low-grade or worsening depression (Earls, 2010), and therefore, infant developmental delays (Deave, Heron, Evans, & Emond, 2008). Moreover, the sensitivity of the EPDS to detect depression is enhanced with a lower symptom threshold (Tandon, Cluxton-Keller, Leis, Le, & Perry, 2012). Our results suggest that a considerable number of women with significant depression symptoms are being missed by MHSs.
We were also interested in patterns of MHS utilization among women with subclinical PTSD symptoms, but found few guidelines for operationalizing subclinical PTSD on the PCL-5. We reasoned that women could meet DSM-5 criteria for PTSD on the PCL-5 by endorsing one reexperiencing symptom, one avoidance symptom, two negative cognition/mood symptoms, and two arousal symptoms, as occurring with “moderate” or greater intensity (≥ 2 per PCL-5 item), equating to a total score of 12 or higher (American Psychiatric Association, 2013; Morland et al., 2007). We subsequently selected a more conservative subclinical cutoff of 20, which yielded a subclinical PTSD group (n = 20) of comparable size to the low-grade depression group (n = 17).
Similar to findings for depression, 63% (n = 19) of women with very elevated clinical PTSD scores (≥ 33; National Center for PTSD, 2019) received MHSs at some point during pregnancy. In contrast, only 40% (n = 8) of women with subclinical PTSD symptoms (scores of 20–32) utilized MHSs during pregnancy. Several studies using DSM-IV criteria have documented that pregnant women with subclinical PTSD symptoms experience considerable distress, impairment, risky health behaviors, and comorbid depression and anxiety (e.g., Onoye et al., 2013). Therefore, it is concerning that so few women with subclinical PTSD symptoms appear to be receiving care.
Overall, there are troubling discrepancies in MHS utilization between women with very elevated versus low-grade depression symptoms, and between women with clinical versus subclinical PTSD symptoms. This difference could indicate that women are only referred for MHSs when they have severe symptoms, even though low-grade or subclinical symptoms put them and their babies at risk. Conservative symptom cut-offs are risky and may miss women who do, in fact, have clinical symptom levels that are not being captured by questionnaires because of minimization/denial, social desirability biases, or language and cultural barriers. Alternatively, pregnant women may only seek MHSs when their depression or PTSD symptoms are severe and can less easily be ignored or attributed to more normative symptoms of pregnancy. In either case, our findings indicate that current strategies of screening and intervention in primary care are failing to serve all women who need mental health care.
Thematic Analysis of Barriers and Solutions to MHS Utilization
Finally, based on interview responses, we sought to understand what factors women personally perceived as barriers to MHS utilization during pregnancy and what recommendations they offered as potential solutions to help them access MHSs. Women who completed the 3–4-month postpartum interview (76%, n = 77) provided responses. (Attrition analyses indicated that the only demographic or mental health-related variable that differentiated women who did versus did not complete the postnatal interview was higher educational attainment, p < .01.)
Barriers
Thematic analysis of participant interviews revealed eight major categories of barriers to MHS utilization (see Figure 2). The most commonly identified barrier was transportation and accessibility of services (31%, n = 20). Many women expressed that they lacked access to affordable, reliable, safe, fast, and convenient transportation to attend appointments. They often noted that San Francisco’s public transportation was crowded and ran late. Several women described particular difficulty in traveling to appointments with their children. One woman encapsulated several of these concerns when she said, “Getting on the bus with three kids costs a lot and takes a lot of effort.” This issue may be exacerbated by ongoing gentrification and displacement of low-income women in the San Francisco Bay Area (Pogash, 2015).

The next most common barrier pertained to parenting demands (19%, n = 12). Women remarked that parenting responsibilities made it difficult to manage and get to appointments. They identified that attending health care appointments was challenging because they lacked child care and had to prioritize their children’s needs (e.g., children getting sick). For example, one woman who worked remarked that it was difficult to make appointments because her availability coincided with times when her children were going to and from school.
Women indicated that it required a great deal of effort to make and keep appointments (11%, n = 7). For example, one woman said, “Getting up and getting there is hard.” Several women suggested that bad weather made traveling to appointments a daunting task. An equally common barrier was the difficulty of managing multiple appointments (11%, n = 7). Women found it difficult to remember when appointments were scheduled and to manage time effectively, especially as many different appointments accumulated (e.g., “trying to make all the other appointments”). Women suggested that other health care appointments were of higher priority and that mental health was a lesser concern than physical health (e.g., “anything that conflicts with a [medical] doctor’s appointment [is less important]”). Scheduling appointments was difficult, because of inflexible work schedules and agencies operating only during business hours (8%, n = 5). Women seemed to have little control over their work schedules and faced competing demands (e.g., “having work scheduled on top of appointments”), or were unable to leave work during the day for an appointment. Even when women were motivated and able to attend appointments, they encountered long wait times, such that it took a long time to get an appointment, and then took a long time for it to begin (6%, n = 4).
Women also noted that health-related challenges, including physical and mental health problems, interfered with their ability to attend appointments (9%, n = 6). Examples included: “being tired during pregnancy,” “morning sickness,” and “my depression.” Finally, there were several other barriers that did not fit into other categories (6%, n = 4).
Solutions
Women generated many ideas about how to improve access to prenatal MHSs. Thematic analysis of the interviews yielded seven major categories of solutions to increase MHS utilization (see Figure 3). Most commonly, suggestions had to do with improving the agency–client relationship (21%, n = 18). Women wished that they were better understood and treated with more respect by service providers, and that agencies would “not judge pregnant women.” Women emphasized the need for service providers to support them and “be a listening ear.” One woman said service providers “could care more… and help out more.” Similarly, women highlighted the need for agencies to function more effectively, with suggestions about providers being on time for appointments and improving communication within the agency.
The other major recommendation for improving MHSs was to provide more comprehensive care and connections to practical resources (18%, n = 15). For example, women expressed that they needed housing, food, child care, and legal services. In general, a theme during the interviews was that concrete needs were higher priority than mental health. Women also suggested that agencies expand pregnancy-related services (11%, n = 9). In other words, agencies could tailor MHSs to be more applicable and relevant for pregnant women, by providing services such as support groups, peer mentorship programs, childbirth preparation classes, and services for expectant fathers. Some women recommended integrated prenatal physical and mental health care (e.g., “Instead of suggesting that [women] go to see a therapist, the doctors could talk to the women themselves”).
Women described a need for increased community knowledge about MHSs and resources available during pregnancy (8%, n = 7). These suggestions included making services “more visible,” increasing clarity about services offered, and doing more community outreach. Women suggested that agencies should find ways to reach people who “have a hard time asking for help” and more proactively ask how women are doing because “if not asked, they won’t tell.”
Finally, many women were unsure about how MHSs could be improved (12%, n = 10). There were several other suggestions for improvement of MHSs that did not map on to other categories (11%, n = 9). On a positive note, some women expressed that they were satisfied with existing services and did not believe that they needed to be improved (11%, n = 9). Several women remarked how appreciative they were of service providers (e.g., “they are doing a lot of good things”). Finally, it is notable that even though transportation and accessibility issues were most commonly listed as barriers, improving accessibility was infrequently raised as a potential solution to increase service access (8%, n = 7), perhaps due to a lack of awareness that resources like ride service or on-site child care could be provided.

Extending the Reach of Prenatal MHSs: Urgent Recommendations for Agencies and Providers
Although the majority (68%) of pregnant women in our sample had very elevated MHS needs, only about half (54%, n = 37) of those women received any MHSs during pregnancy. This low rate of MHS utilization is particularly striking considering that the majority of women in this study were recruited from within a hospital where women were already connected to comprehensive prenatal care. The dramatic gap between prenatal MHS need and utilization signals an imperative for MHS providers and agencies to adapt and innovate to better serve these women.
Fortunately, this study also identified several potential areas for growth in prenatal MHSs. First, we identified several sociodemographic factors associated with MHS utilization among those who had clinical MHS need: being White, being unpartnered, and reporting greater childhood family dysfunction. Although we did not directly assess cultural attitudes toward mental health, it appears that there may be cultural barriers to prenatal MHS utilization among women of color. To better engage women of color in MHSs, it is important for providers to be culturally competent and representative of the populations they serve (Brach & Fraserirector, 2000). Providers might consider asking at intake how women’s cultural backgrounds affect their views on mental health problems and treatment, and integrating these views into treatment approaches and goals. Outreach efforts may also benefit from an emphasis on promoting awareness of not only postpartum, but prenatal, mental health problems and their consequences to the mother and fetus, as well as an effort to combat culturally specific stigma about mental illness and treatment. Given that women are more likely to receive postpartum than prenatal MHSs (Glasheen et al., 2015), agencies and providers could explain or distribute flyers articulating that depression and PTSD are even more common during pregnancy than postpartum (Underwood et al., 2016) and that prenatal mental health problems are particularly risky for the baby. Providers can normalize prenatal mental health problems by explaining that women undergo a tremendous amount of change during pregnancy, helping them identify specific stressors, and reflecting that women need not shoulder these burdens alone. Finally, although outside the scope of the current study, it will be important in future work to examine the intersection of MHS need and utilization among women with unwanted pregnancies. These women may be at high risk of prenatal mental health problems, but also be reluctant to seek services because of ambivalence toward the pregnancy.
Another important observation of this study was that pregnant women with low-grade depression and subclinical PTSD symptoms are unlikely to receive MHSs, despite health risks for women and their babies (Deave et al., 2008; Onoye et al., 2013). Whereas 61–63% of women with very elevated clinical depression symptoms (EPDS ≥ 13) and clinical PTSD symptoms (PCL-5 ≥ 33) received MHSs during pregnancy, only 35–40% of women at the low-grade, AAP-recommended clinical level for depression on the EPDS (≥ 10) and the subclinical level for PTSD on the PCL-5 (≥ 20) received MHSs. This phenomenon calls for two action steps by MHS agencies and providers: (1) increase awareness of mental health problems among pregnant women and (2) widen the net of early clinical screening and intervention.
As noted previously, pregnant women, particularly those of color, may be unfamiliar with the prevalence and risks of prenatal mental health problems, especially those at the low-grade or subclinical level. Some women may not realize that their symptoms exceed the normative mood fluctuations of pregnancy, or may dismiss their symptoms as hormonal and temporary, calling for concerted awareness campaigns. However, it is equally, if not more, important that women with lower (but still elevated) symptom levels are referred for treatment. The risks of failing to treat women with lower symptom levels—who need care because their symptoms are impairing, likely to worsen, or harmful to fetal development—are far greater than the risks of providing services to women who may not truly need them. In service of the goal to detect women with lowgrade or subclinical symptoms, all MHS agencies and primary care physicians should adopt the depression screener (EPDS) cutoff of 10 recommended by AAP, and consider using lower cutoffs for PTSD screeners (e.g., PCL-5 score of 20), and then refer to MHSs all women who meet or exceed these thresholds.
Additional insights for MHS agencies and providers came directly from women themselves, reflecting on how service providers could better care for pregnant women. This line of inquiry is important, given that rates of prenatal mental health treatment are even lower than rates of prenatal mental health assessment (Kelly et al., 2001). It follows that some women may be aware that they have significant mental health symptoms, but still do not pursue or receive treatment.
Agencies and providers can improve services to address the barriers and solutions articulated by our research participants. The primary recommendation from women was to improve the agency–client relationship. Women emphasized the need for providers to be supportive, nonjudgmental, respectful, and understanding, so that women could fully benefit from prenatal services. This point is underscored by lessons we learned during the process of conducting this study: Although not a treatment study, we endeavored to cultivate a trusting relationship with participants and, in turn, women reported therapeutic benefit from participation. The therapeutic interview model for research, described in Narayan et al. (2017), may also be successful as a prenatal MHS intake procedure that promotes service engagement and retention by building rapport and trust, emphasizing strengths, promoting awareness of stressors, and personally/orally asking about symptoms (rather than using impersonal paper/pencil- or computer-administered screeners to collect data). In our study, we regularly observed that following these rapport-building techniques, women were very willing to be open and share their experiences, and then they were receptive to the suggestion of MHSs when indicated. Moreover, interventions to support rapport-building and compassionate care often take the form of caring for those who care. Interventions that address provider burnout and compassion fatigue increase empathy and bolster the capacity of service providers to tolerate vicarious exposure to trauma and adversity (Wilkinson, Whittington, Perry, & Eames, 2017).
Agency- and provider-level solutions can also address practical barriers and needs that participants described. Women noted that they faced considerable challenges related to transportation, child care, and scheduling, and that MHSs should be more comprehensive and relevant to the perinatal period. Based on their recommendations, we believe that a model of integrated prenatal care and case management would be beneficial. Under an integrated model, women could access services for prenatal care, physical health, mental health, housing, food, and legal aid in one place, increasing the likelihood that women receive relevant, high-quality referrals that are easy to pursue. Centralized models also enhance the capacity of providers to coordinate screening, referral, and follow-up of services for high-risk patients, ensuring that clients do not “fall through the cracks.” To better tailor services to the perinatal period, offerings could include support groups for pregnant women, peer mentor programs, childbirth preparation classes, and psychosocial services for fathers. In addition, logistical supports, such as subsidizing or providing transportation and child care, are critical to allow women to benefit from services. Creative care models that “meet women where they are” can also address the burden of service coordination for busy mothers who may have limited job security and flexibility. For instance, home visiting, community health promoter models, and mobile/text-based interventions can reduce barriers and personalize care (Evans et al., 2015; Maravilla, Betts, Abajobir, Couto e Cruz, & Alati, 2016). Finally, it seems that appointment reminders, flexible scheduling, drop-in appointments, and appointments outside of typical business hours would also be helpful strategies.
In closing, with increased contact between women and the health care system during pregnancy, there is unrivaled opportunity to detect and successfully intervene upon women’s prenatal mental health problems. MHS providers have already made great strides in their efforts to screen and treat pregnant women with mental illness, reflected by the comments of several women who recognized and appreciated the services they already received. Nevertheless, there remains room for growth in prenatal MHS delivery to extend the reach of services to a wider net of distressed women. In so doing, MHS providers have the ability to promote healthier trajectories for new mothers and their infants, beginning as early in development as possible.
Learn More
Trauma Informed Care in the Perinatal Period
J. Seng & J. Taylor (Eds.) (2015)
Edinburgh, Scotland: Dunedin Academic Press
Survivor Moms: Women’s Stories of Birthing, Mothering and Healing After Sexual Abuse
M. Sperlich & J. S. Seng (2008)
Eugene, OR: Motherbaby Press
Perinatal and Postpartum Mood Disorders: Perspectives and Treatment Guide for the Health Care Practitioner
S. D. Stone & A. E. Menken (Eds.) (2008)
New York, NY: Springer Publishing Company
Counseling the Culturally Diverse: Theory and Practice (6th ed.)
D. W. Sue & D. Sue (Eds.) (2013)
Hoboken, NJ: John Wiley & Sons
About the Authors
Laura M. River, MA, is a doctoral student in clinical child psychology at the University of Denver. She completed her bachelor’s degree in psychology at Pomona College and her master’s degree in clinical child psychology at the University of Denver. Her research focuses on factors that promote sensitive parenting and child well-being, with particular interest in how interventions targeting prenatal mental health and romantic relationship quality might strengthen the emerging parent– child relationship.
Angela J. Narayan, PhD, is an assistant professor in the clinical child psychology doctoral program at the University of Denver, and an assistant adjunct professor in the Department of Psychiatry at the University of California, San Francisco (UCSF). She completed her doctoral training in clinical child psychology at the Institute of Child Development, University of Minnesota, and her postdoctoral training at the Child Trauma Research Program within the Department of Psychiatry at UCSF. Her research focuses on developmental psychopathology, childhood trauma, perinatal and infant mental health, and resilience. One of her current research directions focuses on understanding how the prenatal period is a key turning point to buffer the intergenerational transmission of risk in pregnant women and fathers-to-be with histories of childhood trauma, and how to promote resilience in parents and infants.
Thania Galvan, MA, is a doctoral student in clinical child psychology at the University of Denver. She completed her bachelor’s degree in psychology at Trinity University and her master’s degree in clinical child psychology at the University of Denver. Her research focuses on examining mechanisms that contribute to and/or maintain mental health disparities among underserved populations, with a particular interest in working with Latinx populations.
Luisa Rivera, MPH, researches the biological embedding of early life stress and the intergenerational effects of social adversity. She completed her public health graduate training at the University of Minnesota specializing in maternal and child health. A trained doula, she is passionate about expanding access to perinatal mental health treatment, especially for immigrant families and communities of color. She is currently pursuing her doctorate in anthropology at Emory University.
William W. Harris, PhD, received a bachelor’s in psychology from Wesleyan University and a doctorate in urban studies from the Massachusetts Institute of Technology. In 1981, Harris founded KidsPac, a political action committee dedicated to public policies for poor children from birth to 6 years old, and in 1984, Harris founded Children’s Research and Education Institute. He speaks and teaches frequently about children and politics at universities, political gatherings, and public policy fora. He is an adjunct professor in the Department of Psychiatry at the University of California, San Francisco.
Alicia F. Lieberman, PhD, is a professor in the University of California, San Francisco (UCSF) Department of Psychiatry, Irving B. Harris Endowed Chair in Infant Mental Health, vice chair for academic affairs, and director of the UCSF Child Trauma Research Program. She is past president and former member of the board of directors of ZERO TO THREE, and is on the board of trustees of the Irving Harris Foundation. She is currently the director of the Early Trauma Treatment Network, a center of the Substance Abuse and Mental Health Services Administration National Child Traumatic Stress Network that consists of a collaborative of four university sites that include the UCSF/San Francisco General Hospital Child Trauma Research Program, Boston Medical Center, Louisiana State University Medical Center, and Tulane University.
Suggested Citation
River, L. M., Narayan, A. J., Galvan, T., Rivera, L., Harris, W. W., & Lieberman, A. F. (2019). On the verge of motherhood and mental illness: Prenatal mental health service utilization among women at highest risk. ZERO TO THREE Journal, 39(5), 33–42.
References
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Arlington, VA: American Psychiatric Publishing.
Brach, C., & Fraserirector, I. (2000). Can cultural competency reduce racial and ethnic health disparities? A review and conceptual model. Medical Care Research and Review, 57(1_suppl), 181–217. doi:10.1177/1077558700057001s09
Centers for Disease Control and Prevention. (2016). Adverse childhood experiences (ACEs). Source link
Choi, K. W., & Sikkema, K. J. (2016). Childhood maltreatment and perinatal mood and anxiety disorders: A systematic review. Trauma, Violence, & Abuse, 17(5), 427–453. doi: 10.1177/1524838015584369
Cook, C. A. L., Flick, L. H., Homan, S. M., Campbell, C., McSweeney, M., & Gallagher, M. E. (2010). Psychiatric disorders and treatment in low-income pregnant women. Journal of Women’s Health, 19(7), 1251–1262. doi:10.1089/jwh.2009.1854
Cox, J. L., Holden, J. M., & Sagovsky, R. (1987). Detection of postnatal depression: Development of the 10-item Edinburgh Postnatal Depression Scale. The British Journal of Psychiatry, 150(6), 782–786. doi: 10.1192/ bjp.150.6.782
Deave, T., Heron, J., Evans, J., & Emond, A. (2008). The impact of maternal depression in pregnancy on early child development. BJOG: An International Journal of Obstetrics & Gynaecology, 115(8), 1043–1051. doi:10.1111/j.1471-0528.2008.01752.x
Earls, M. F. (2010). Incorporating recognition and management of perinatal and postpartum depression into pediatric practice. Pediatrics, 126(5), 1032–1039. doi: 10.1542/peds.2010-2348
Evans, W., Nielsen, P. E., Szekely, D. R., Bihm, J. W., Murray, E. A., Snider, J., & Abroms, L. C. (2015). Dose-response effects of the Text4baby Mobile Health Program: Randomized controlled trial. JMIR mHealth and uHealth, 3(1), e12. doi: 10.2196/mhealth.3909
Glasheen, C., Colpe, L., Hoffman, V., & Warren, L. K. (2015). Prevalence of serious psychological distress and mental health treatment in a national sample of pregnant and postpartum women. Maternal and Child Health Journal, 19(1), 204–216. doi: 10.1007/s10995-014-1511-2
Kelly, R. H., Zatzick, D. F., & Anders, T. F. (2001). The detection and treatment of psychiatric disorders and substance use among pregnant women cared for in obstetrics. American Journal of Psychiatry, 158(2), 213–219. doi: 10.1176/appi.ajp.158.2.213
Lancaster, C. A., Gold, K. J., Flynn, H. A., Yoo, H., Marcus, S. M., & Davis, M. M. (2010). Risk factors for depressive symptoms during pregnancy: A systematic review. American Journal of Obstetrics and Gynecology, 202(1), 5–14. doi:10.1016/j.ajog.2009.09.007
Lieberman, A. F., Diaz, M. A., & Van Horn, P. (2009). Safer beginnings: Perinatal Child-Parent Psychotherapy for newborns and mothers exposed to domestic violence. ZERO TO THREE Journal, 29(5), 17–22.
Maravilla, J. C., Betts, K. S., Abajobir, A. A., Couto e Cruz, C., & Alati, R. (2016). The role of community health workers in preventing adolescent repeat pregnancies and births. Journal of Adolescent Health, 59(4), 378–390. Source link.
Morland, L., Goebert, D., Onoye, J., Frattarelli, L., Derauf, C., Herbst, M., … Friedman, M. (2007). Posttraumatic stress disorder and pregnancy health: Preliminary update and implications. Psychosomatics, 48(4), 304–308. doi: 10.1176/appi.psy.48.4.304
Narayan, A. J., Rivera, L. M., Bernstein, R. E., Castro, G., Gantt, T., Thomas, M., Nau, M., Harris, W. W., & Lieberman, A. F. (2017). Between pregnancy and motherhood: Identifying unmet mental health needs in pregnant women with lifetime adversity. ZERO TO THREE Journal, 37(4), 14–23.
Narayan, A. J., Rivera, L. M., Bernstein, R. E., Harris, W. W., & Lieberman, A. F. (2018). Positive childhood experiences predict less psychopathology and stress in pregnant women with childhood adversity: A pilot study of the benevolent childhood experiences (BCEs) scale. Child Abuse & Neglect, 78, 19–30. doi: 10.1016/j.chiabu.2017.09.022
National Center for PTSD. (2019). PTSD Checklist for DSM-5 (PCL-5). Source link
Onoye, J. M., Shafer, L. A., Goebert, D. A., Morland, L. A., Matsu, C. R., & Hamagami, F. (2013). Changes in PTSD symptomatology and mental health during pregnancy and postpartum. Archives of Women’s Mental Health, 16(6), 453–463. doi: 10.1007/s00737-013-0365-8
Pogash, C. (2015, May 22). Gentrification spreads an upheaval in San Francisco’s Mission District. The New York Times. Source link
Seng, J. S., Rauch, S. A., Resnick, H., Reed, C. D., King, A., Low, L. K., … & Liberzon, I. (2010). Exploring posttraumatic stress disorder symptom profile among pregnant women. Journal of Psychosomatic Obstetrics & Gynecology, 31(3), 176–187. doi: 10.3109/0167482x.2010.486453
Seng, J. S., Sperlich, M., Low, L. K., Ronis, D. L., Muzik, M., & Liberzon, I. (2013). Child abuse history, posttraumatic stress disorder, post-partum mental health, and bonding: A prospective cohort study. Journal of Midwifery & Women’s Health, 58(1), 57–68. doi:10.1111/j.1542-2011.2012.00237.x
Slade, A., Cohen, L. J., Sadler, L. S., & Miller, M. (2009). The psychology and psychopathology of pregnancy. In C. H. Zeanah, Jr. (Ed.), Handbook of infant mental health (pp. 22–39). New York, NY: Guilford Press.
Tandon, S. D., Cluxton-Keller, F., Leis, J., Le, H.-N., & Perry, D. F. (2012). A comparison of three screening tools to identify perinatal depression among low-income African American women. Journal of Affective Disorders, 136(1–2), 155–162. doi: 10.1016/j.jad.2011.07.014
Underwood, L., Waldie, K., D’Souza, S., Peterson, E. R., & Morton, S. (2016). A review of longitudinal studies on antenatal and postnatal depression. Archives of Women’s Mental Health, 19(5), 711–720. doi: 10.1007/s00737-016-0629-1
Vanderkruik, R., Lemon, E., River, L. M., & Dimidjian, S. (in press). Perinatal depression. In C. S. Richards & L. M. Cohen (Eds.), The Wiley encyclopedia of health psychology vol. III: Clinical health psychology and behavioral medicine. Hoboken, NJ: John Wiley & Sons.
Vesga-López, O., Blanco, C., Keyes, K., Olfson, M., Grant, B. F., & Hasin, D. S. (2008). Psychiatric disorders in pregnant and postpartum women in the United States. Archives of General Psychiatry, 65(7), 805–815. doi: 10.1001/archpsyc.65.7.805
Weathers, F. W., Litz, B. T., Keane, T. M., Palmieri, P. A., Marx, B. P., & Schnurr, P. P. (2013). The PTSD Checklist for DSM-5 (PCL-5). Scale available from the National Center for PTSD at www.ptsd.va.gov
Wilkinson, H., Whittington, R., Perry, L., & Eames, C. (2017). Examining the relationship between burnout and empathy in healthcare professionals: A systematic review. Burnout Research, 6, 18–29. doi: 10.1016/j.burn.2017.06.00