PERSPECTIVES: Reflections From the Field: The Role of Occupational Therapy After Perinatal Loss

Abstract
Perinatal loss (PNL) is considered the loss of any pregnancy or infant from the time of conception up until 1 year after a woman delivers. One in 4 women will experience PNL while 1 in 3 women will experience perinatal mood disorders such as anxiety, depression, and/or posttraumatic stress disorder whether they experience a healthy pregnancy and delivery or experience PNL. In this article, authors describe variable aspects to current processes of care related to PNL. The authors describe the potential value of occupational therapy in supporting mothers who are parenting after PNL and discuss how a diverse group of providers could contribute to supporting mothers and families with unmet need for services following PNL.
Perinatal loss (PNL) is any loss of a pregnancy or infant and includes miscarriage, termination for medical reasons, stillbirth, neonatal death, and sudden infant death syndrome (Côté- Arsenault et al., 2019). PNL continues to be prevalent in the US. In 2016, infant, neonatal, and post neonatal mortality rates as a total were reported as 5.87 per 1,000 births (Ely et al., 2018). Per the American College of Obstetricians and Gynecologists, 1 in 3 pregnancies end in miscarriages (Wilcox et al., 1988).
A common result of PNL is the diagnosis of perinatal mood and anxiety disorders (PMADs; Kendig et al., 2017). The impact of PMADs and PNL on the quality of life and overall functioning of mothers is long-lasting and significant (Hanish et al., 2019).
Perinatal depression is one of the most common complications of pregnancy and postpartum, affecting 1 out of 7 mothers in the United States (Kendig et al., 2017). Perinatal anxiety disorders impact 11% to 21% of mothers every year (Kendig et al., 2017). Perinatal depression and anxiety disorders have been shown to link to negative perinatal outcomes that will impact mothers, parents, and infants. Perinatal post-traumatic stress disorder (P-PTSD) can also arise after traumatic experiences, occurring from conception to 6 months postpartum (Cirino & Knapp, 2019). Given that childbirth itself can be a traumatic experience and a possible cause of P-PTSD, it is important to recognize the complex trauma that is associated with PNL (Cirino & Knapp, 2019). PNL affects multiple areas of mother’s lives including self-care, activities of daily living, social engagement, and other meaningful occupations and roles of the individual (Hanish et al., 2019).
Current Processes of Care Related to PNL
The current process of care is often fragmented and varied for mothers who experience PNL and subsequent sequalae, such as PMADs and occupational imbalance. Further, the quality and level of care is not standardized across settings and across the health care system in the US (Sepulveda, 2019). Prior to pregnancy, many mothers who experience PNL are not aware that it is a possible and common outcome. Often, these individuals are informed of the risk of PNL only following its occurrence. Furthermore, individuals of various identities, backgrounds, and levels of privilege will experience varied levels of care depending on the type of PNL, the environments they have access to, and the quality of health care professionals and resources available to them (Cacciatore & Bushfield, 2007; Hanish et al., 2019).
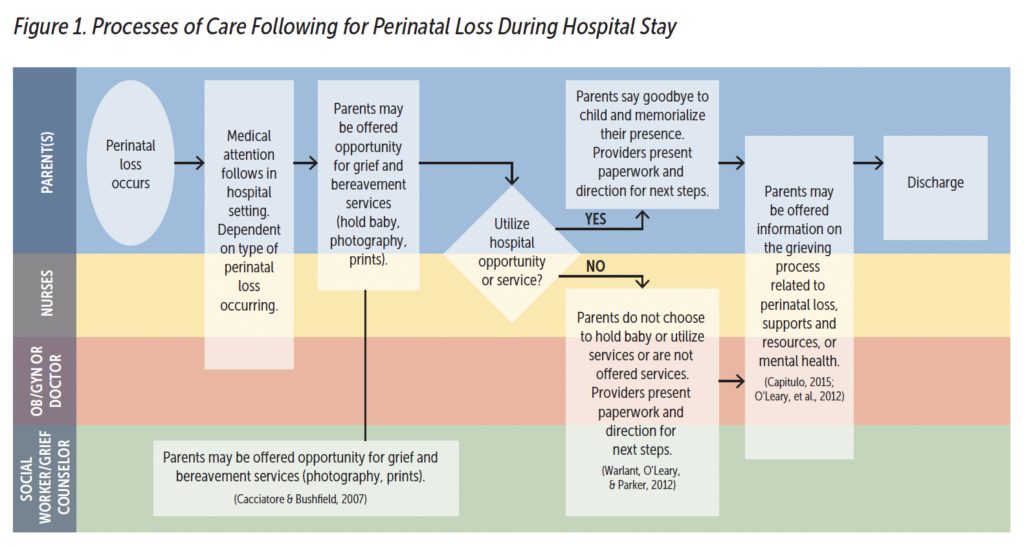
Mothers who experience loss are often processing much of the grief and trauma alone due to the fragmented processes of care related to PNL. Seeking out and securing support and services can delay the immediate care necessary for addressing the challenges that mothers might experience after loss. Therefore, it is important to recognize the gaps and areas of needed improvement (Cacciatore & Bushfield, 2007; Capitulo, 2005). Promptly following the occurrence of PNL, mothers are first typically provided immediate care to stabilize their medical condition. Depending on their setting, mothers may then be offered hospital services to process loss. Parents may be provided a chance to say goodbye or create memories with their child through photography, memory box making, or making hand and footprints, or proceed directly to discharge (see Figure 1).
Following hospital discharge, mothers will receive follow-up care, which varies depending on when the loss occurred. If the loss is recent, the mother may receive grief and bereavement service or resources following immediate medical care (Cacciatore & Bushfield, 2007). If time has passed since the loss, follow-up will take place in a primary care setting with a generic mental health evaluation to assess overall mental health. There may be recommendations for support groups or other mental health referrals based on the results of the screener. Whether mothers are informed of grief and mental health supports varies depending on their individual context and environment. Commonly, individuals find PNL support groups or therapists through social networks.

Diversifying the Health Care Team
Health care providers need to understand the impact of PNL on mothers’ overall functioning and well-being. The professionals who most commonly work with this population include obstetricians/gynecologists, nurses, midwives, and social workers. It is imperative that these professionals and other health providers who work with birthing parents are adequately prepared. A mother’s mental health following loss will impact her ability to participate in valued routines and can potentially limit social interactions, health management, and parenting and caregiving (Hanish et al., 2019). Therefore, health care providers should know about local mental health providers and other resources to whom they can refer mothers. In addition, health care providers need a trauma- and culturally informed perspective when supporting a mother after PNL (Cacciatore & Bushfield, 2007) in order to better direct their clients to access the appropriate support and resources.
The Role of Occupational Therapy
Occupational therapists can contribute to improving the processes of care around PNL by delivering individualized and holistic interventions that consider how a given experience has impacted a client’s ability to perform and participate within their valued routines (i.e., occupations; Occupational Therapy Practice Framework: Domain and Process—Fourth edition [OTPF-4], 2020). These areas of occupation include health management, social participation, activities of daily living, and leisure (OTPF-4, 2020). Occupational therapists are skilled at considering how a mother’s mental health following loss could impact her current and desired occupational profile in this context.
Return to Zero: HOPE
An example of an occupational therapy-led organization that supports the PNL community and provides educational opportunities for health care professionals is the national non-profit organization Return to Zero: HOPE (RTZ HOPE). Their occupation-based retreats have helped bereaved mothers process their grief and symptoms related to anxiety, depression, and trauma as well as assisted in creating a peer-to-peer support system (Hanish et al., 2019). The scope of supports provided by RTZ HOPE include:
- interventions tailored with the understanding of grief and mental health impacting performance and participation,
- parent coaching for mother and child attachment and sibling-to-sibling attachment,
- groups to facilitate processing of grief and perceptions of parenting after loss, and
- parent coaching for mothers parenting after loss to address co-regulation and transitions.
While RTZ HOPE and other organizations have resources and recommendations on what services to offer, they recognize the need to expand on the resources available to mothers who experience loss to increase access to services and resources. Evidence-based tools are necessary to direct and connect clients to resources and close the gaps within the processes of care related to PNL. For example, providers could benefit from a checklist tool to more efficiently and effectively address the needs of the mother given how much of loss story she has processed. This checklist would also tell providers how the loss has impacted the mother’s ability to participate in routines individual to herself and that of her family which would then impact her participation and performance in her role as a caregiver. This type of work is consistent with the call for occupational therapists to screen for and treat mothers for P-PTSD while working with the child and their family, including children and families accessing early intervention settings and those from historically minoritized backgrounds (Pizur- Barnekow & Erickson, 2011; Rao, 2022).
Conclusion
Mothers who parent after PNL require intervention that is individually tailored to their evolving needs. A diversified health care team is equipped to understand the impact of loss on mothers and provide tailored support. Occupational therapists can play a unique role in helping mothers return to performing and participating in meaningful activities and roles in daily life. As occupational therapists are recognizing their contribution to health care teams, their skilled support for the PNL community can close the gap in process of care following PNL. The development of evidence-based tools, such as checklists to better screen for unmet need, can further enhance their skilled contribution within this community.
Acknowledgment
This article was drafted in partial fulfillment of post-professional occupational therapy doctorate degree requirements at the University of Illinois Chicago (A. Rao) and is dedicated to Dr. Arameh Anvarizadeh: Thank you for your continued support as I pursue my professional journey with your efforts for equity and access as inspiration to create just that for mothers who have experienced loss.
Asha Rao, OTD, OTR/L, (she/her/hers) is a pediatric occupational therapist practicing in early intervention through her company, Adaptations Unlimited, in the suburbs of Northern Illinois. Dr. Rao completed her bachelor’s degree in rehabilitation sciences, her master’s degree in occupational therapy, and her post-professional occupational therapy doctorate (OTD). Dr. Rao’s OTD focused on occupational therapy’s role in supporting mothers parenting after loss. Outside of clinical practice, Dr. Rao advocates for disability in South Asian communities as co-editor for Brown Girl Magazine and is a courier co-editor for COTAD (Coalition of Occupational Therapy Advocates for Diversity).
Kiley Hanish, OTD, OTR/L, is an occupational therapist specializing in mental health during pregnancy and the postpartum period. She received her bachelor of arts degree from Loyola Marymount University, and masters and doctoral degrees in occupational therapy from the University of Southern California. Dr. Hanish currently serves in the position of assistant professor in the Occupational Therapy Doctorate program at Keck Graduate Institute, teaching psychosocial occupational therapy. She looks forward to sharing her expertise about perinatal mental health, grief, and loss through inter-professional collaboration within the KGI community. Dr. Hanish is the founding director of the nonprofit organization Return to Zero: HOPE, where she advocates for and guides bereaved families in reclaiming their purpose and meaning after the tragic loss of their child.
Mary A. Khetani, ScD, OTR/L, FAOTA, (she/her/hers) is a pediatric occupational therapist and rehabilitation scientist. Dr. Khetani is currently a professor in the University of Illinois Chicago Department of Occupational Therapy and directs the Children’s Participation in Environment Research Lab (CPERL; cperl.ahs.uic.edu). CPERL pursues innovative childhood disability research and knowledge translation activities, inclusive of partnership with the CanChild Centre for Childhood Disability Research in Canada. Dr. Khetani was a member of the ZERO TO THREE Fellows class of 2007–2009.
Heidi Fischer, OTD, OTR/L, is a clinical associate professor in occupational therapy at the University of Illinois at Chicago. She earned a bachelor of science degree in psychology at the University of Illinois at Urbana-Champaign and master of science degree and her doctorate in occupational therapy from the University of Illinois at Chicago. Dr. Fischer serves as director of the University of Illinois at Chicago Occupational Therapy Faculty Practice: Self-Management for People With Chronic Conditions, where she provides occupational therapy services to people experiencing diabetes. Dr. Fischer is co-investigator for two federally funded research grants and is co-author of more than 45 articles and 3 book chapters, and she has presented at more than 50 national and international conferences. Prior to University of Illinois at Chicago, Dr. Fischer was an occupational therapist and clinical research coordinator at the Shirley Ryan AbilityLab and served as quality consultant for the American Occupational Therapy Association.
Suggested Citation
Rao, A., Hanish, K., Khetani, M., & Heidi Fischer, H. (2023). PERSPECTIVES: Reflections from the field—The role of occupational therapy after perinatal loss. ZERO TO THREE Journal, 43(4), 46-49.
References
Cacciatore, J., & Bushfield, S. (2007). Stillbirth: The mother’s experience and implications for improving care. Journal of Social Work in End-Of-Life & Palliative Care, 3(3), 59–79. https://doi.org/10.1300/j457v03n03_06. www.tandfonline.com/doi/abs/10.1300/J457v03n03_06
Capitulo, K. L. (2005). Evidence for healing interventions with perinatal bereavement. MCN, The American Journal of Maternal/Child Nursing, 30(6), 389–396. https://doi.org/10.1097/00005721-200511000-00007. https://journals.lww.com/mcnjournal/Abstract/2005/11000/Evidence_for_Healing_Interventions_With_Perinatal.7.aspx
Cirino, N., & Knapp, J. (2019). Perinatal posttraumatic stress disorder: A review of risk factors, diagnosis, and treatment. Obstetrical & Gynecological Survey, 74(6), 369–376. doi: 10.1097/OGX.0000000000000680. https://journals.lww.com/obgynsurvey/Abstract/2019/06000/Perinatal_Posttraumatic_Stress_Disorder__A_Review.20.aspx
Côté-Arsenault, D., Leerkes, E. M., & Zhou, N. (2019). Individual differences in maternal, marital, parenting and child outcomes following perinatal loss: A longitudinal study. Journal of Reproductive and Infant Psychology, 38(1), 3–15. https://doi.org/10.1080/02646838.2019.1579897. www.tandfonline.com/doi/abs/10.1080/02646838.2019.1579897?journalCode=cjri20
Ely, D. M., Driscoll, A. K., & Matthews, T. G. (2018). Infant mortality by age at death in the United States, 2016. PubMed, 326, 18. https://pubmed.ncbi.nlm.nih.gov/30475688
Hanish, K. K., Margulies, I., & Cogan, A. M. (2019). Evaluation of an occupationbased retreat for women after pregnancy or infant loss. The American Journal of Occupational Therapy, 73(5), 7305345030p1-7305345030p6. https://doi.org/10.5014/ajot.2019.034025. https://research.aota.org/ajot/article-abstract/73/5/7305345030p1/9864/Evaluation-of-an-Occupation-Based-Retreat-for?redirectedFrom=fulltext
Kendig, S., Keats, J. P., Hoffman, M. C., Kay, L. B., Miller, E. S., Moore Simas, T. A., Frieder, A., Hackley, B., Indman, P., Raines, C., Semenuk, K., Wisner, K. L., & Lemieux, L. A. (2017). Consensus bundle on maternal hental Health. Obstetrics & Gynecology, 129(3), 422–430. https://doi.org/10.1097/aog.0000000000001902. https://journals.lww.com/greenjournal/Fulltext/2017/03000/Consensus_Bundle_on_Maternal_Mental_Health_.4.aspx
Occupational Therapy Practice Framework: Domain and Process—Fourth edition (OTPF-4). (2020). The American Journal of Occupational Therapy, 74(Supp. 2), https://doi.org/10.5014/ajot.2020.74s2001. https://research.aota.org/ajot/article-abstract/74/Supplement_2/7412410010p1/8382/Occupational-Therapy-Practice-Framework-Domainand?redirectedFrom=fulltext
O’Leary, J., & Warland, J. (2012). Childbirth preparation for families pregnant after loss. International Journal of Childbirth Education, 27(2), 44+. www.thefreelibrary.com/Childbirth+preparation+for+families+pregnant+after+loss.-a0302298465
Pizur-Barnekow, K., & Erickson, S. (2011). Perinatal post-traumatic stress disorder: Implications for occupational therapy in early intervention practice. Occupational Therapy in Mental Health, 27(2), 126–139. DOI: 10.1080/0164212X.2011.566165. www.tandfonline.com/doi/abs/10.1080/0164212X.2011.566165
Rao, A. (2022) Pregnancy and infant loss in South Asian communities. Brown Girl Magazine. https://browngirlmagazine.com/pregnancy-infant-loss
Sepulveda, A. A. (2019). A call to action: Addressing maternal mental health in pediatric occupational therapy practice. Annals of International Occupational Therapy, 2(4), 195–200. https://doi.org/10.3928/24761222-20190813-02. https://journals.healio.com/doi/10.3928/24761222-20190813-02
Warland, J., O’Leary, J., & Parker, L. (2012). Intentional parenting of children born after a perinatal loss. Journal of Loss and Trauma, 17(2), 137–157. https://doi.org/10.1080/15325024.2011.595297. www.tandfonline.com/doi/abs/10.1080/15325024.2011.595297
Wilcox, A. J., Weinberg, C. R., O’Connor, J. J., Baird, D. T., Schlatterer, J., Canfield, R. C., Armstrong, E. G., & Nisula, B. C. (1988). Incidence of early loss of pregnancy. The New England Journal of Medicine, 319(4), 189–194. https://doi.org/10.1056/nejm198807283190401. www.nejm.org/doi/full/10.1056/NEJM198807283190401

