Margo Candelaria, University of Maryland School of Social Work, Institute for Innovation and Implementation
Ken Tellerman, Baltimore, Maryland
Anna Maria Wilms Floet, Kennedy Krieger Institute, Johns Hopkins School of Medicine
Heather Whitty, University of Maryland School of Social Work, Institute for Innovation and Implementation
Abstract
Developmental coaching performed by pediatric providers is a first-line, universal relational health promotion intervention. Separate, dedicated, developmental coaching through telehealth complements well-child visits by creating a more relaxed platform. These sessions address parent developmental concerns, allowing space for parent reflection and enhancing parent skills through dialogue and guided practice. The TREEHOUSE program, an outgrowth of the Grow Your Kids: TREE (Talk Read Engage Encourage) program developed by the Maryland Chapter Academy of Pediatrics in 2015, incorporates telehealth developmental coaching into pediatric primary care. Preliminary findings of this Health Resources & Services Administration–funded project indicate successful implementation with providers and positive feedback.
The TREEHOUSE (Talk Read Engage Encourage) program is a first-line universal intervention that fosters health equity in underserved communities by helping to address systemic gaps in the delivery of early intervention (EI) services, including those who may not be eligible for EI services under Part C and Part B section 619 of the Individuals With Disabilities Education Act. The program, developed by the Maryland Chapter American Academy of Pediatrics (MDAAP), promotes positive parent– child interactions through dedicated developmental 30-minute telehealth coaching sessions delivered at ages 9 and 15 months by pediatric practitioners in addition to their routine well-child visits.
Poverty, toxic stress, or other adverse childhood experiences (ACEs) have long-term impacts on brain development and future functioning (Center on the Developing Child, 2019; Felitti et al., 1998). Poverty alone is a known risk factor for developmental delay (Brockmeyer-Cates et al., 2016; Hart & Risley, 1995; Needlman et al., 2005; R. Shah et al., 2015) and children living in poverty face ACEs that affect their cognitive and social–emotional development (Bucci et al., 2016; Garner & Waajid, 2012; Johnson et al., 2013; National Research
Council & Institute of Medicine, 2000; Shonkoff, 2014). The first 5 years of development set the foundation for future social–emotional development, success in school, health, and well-being (National Research Council & Institute of Medicine, 2000). Given the intergenerational impacts of poverty and other ACEs, many caregivers experiencing poverty may themselves have had limited exposure to strategies to promote attachment and resilience (Shonkoff et al., 2012). Parental ACEs have a significant association with developmental delays in their children (Folger et al., 2018).
Children under 2 years old are at a critically sensitive time developmentally. They are at the height of neuroplasticity and greatly benefit from developmentally stimulating experiences and positive caregiver interactions (Center on the Developing Child, 2016). Programs targeting improved parent–child interactions can ameliorate the long-term impact of early parenting and developmental risks, with positive nurturing helping mitigate against the detrimental effects of ACEs and promoting positive development to prevent later negative outcomes for children (Center on the Developing Child, 2016; Gross et al., 2009; National Research Council & Institute of Medicine, 2000; Sheely-Moore & Bratton, 2010; Weisleder et al., 2016).
Despite evidence for effective interventions, there are gaps in the array of infant and early childhood services with many children not receiving needed screening, diagnoses, or treatment (Horwitz et al., 2012; Lipkin et al., 2020). There are insufficient infant and early childhood programs and a shortage of properly trained professionals across diverse settings—primary/specialty medical settings, social services, EI—creating barriers to effective identification and care. Caregivers often turn to infant and early childhood professionals, including pediatric providers, who may not be sufficiently trained to address developmental and behavioral health needs (Freed et al., 2009), with concerns often overlooked (Hebbeler et al., 2007). Primary care providers often refer to subspecialists (e.g., in neurodevelopment, developmental/behavioral pediatrics, psychiatry), who have documented national provider shortages (American Board of Pediatrics, 2018), indicating needed increases in primary care capacity.
Furthermore, screening for ACEs, poverty, and development in pediatric primary care is important but not sufficient. One third of children who are eligible for EI services due to developmental concerns are not referred, and up to two thirds who are referred never make it to their EI evaluation (Jimenez et al., 2014), indicating gaps in identification and referral. In one study, among 2-year old children who did not qualify for EI, approximately 24% had poor academic or behavioral outcomes at school entry. However, parenting behaviors and expectations between 9 months and 3–4 years old were found to possibly mitigate the steep socioeconomic gradient seen in cognitive development at the time of kindergarten entry (Nelson et al., 2016), indicating parenting interventions can target this gap. Primary care providers can use proactive strategies that reduce the impact of adverse experiences and promote resilience in children and families (Traub & Boynton-Jarrett, 2017).

Children under 2 years old are at a critically sensitive time developmentally.
Interventions Within Pediatric Primary Care
Pediatric providers are the ideal professionals to address these gaps in identification and referral. Pediatric providers are a primary resource for parents, particularly during the first 2 years of life when the recommended well-child visit schedule suggests frequent visits (Hagan et al., 2017; Williams et al., 2019). Pediatric providers are among the few professionals who, on a large scale, see families with infants repeatedly over time. Pediatric health care providers and their national organizations are working toward initiatives that prevent and mitigate the effects of poverty (Fierman et al., 2016). In addition, primary care interventions have been demonstrated to mitigate the effects of family poverty on child development (Brockmeyer-Cates et al., 2016).
Promoting Early Relational Health
Moreover, AAP has published a policy statement emphasizing the centrality of relationships in pediatric care and promoting universal interventions within pediatric care as the primary prevention level to promote relational health in families (Garner et al., 2021). Therefore, promoting positive parent–child interactions in pediatrics is an ideal approach because it centers relational health for the family as the conduit to facilitating healthy child development. The ZERO TO THREE Millennial Connections Findings Parent Survey (ZERO TO THREE, 2018) also recommended identifying trusted, community-based partners that can share parenting guidance, such as early childhood professionals, including health care providers.
However, there is a need to go beyond just screening in primary care in order to promote relational health. Parenting interventions that include talking, reading, and playing with young children have been demonstrated to lead to improved developmental outcomes (Ginsburg et al., 2007; Hart & Risley, 1995; High, 2014; Leffel & Suskind, 2013; Milteer et al., 2012; Needlman et al., 2005; P. Shah et al., 2016; Tamis-LeMonda et al., 2001, 2004). Play is noted to be critical in facilitating parent engagement; promoting safe, stable, and nurturing relationships; encouraging the development of numerous competencies, including executive functioning skills; and improving life course trajectories (Lillard et al., 2013), leading to the AAP endorsement of a Prescription for Play at well-child encounters (Yogman et al., 2018).
Developmental Coaching
Developmental coaching presents an opportunity for pediatric primary care practitioners to extend their services beyond surveillance and screening and provide primary prevention to close the developmental gap of children living in poverty and promote relational health. Coaching, as differentiated from teaching and counseling, entails a collaborative process of observation, action and practice, reflection, and feedback (Rush & Shelden, 2020). Developmental coaching is difficult to perform during well-child encounters because a wide array of agenda items often leave little time for teaching parents about child development. Numerous studies have demonstrated telehealth’s feasibility and a high level of satisfaction from patients, families, and providers (Olson et al., 2018). Telehealth developmental coaching visits at home have multiple advantages. Sessions are more relaxed rather than squeezed into a frenetic office visit. Families are generally more relaxed in their home environment. Pediatric providers can observe parent–child interactions and perform developmental surveillance in a more naturalistic setting across developmental domains. Telehealth creates a novel opportunity for the pediatric provider, parents, community visiting nurses, or early intervention specialists to meet online simultaneously. The virtual platform also allows trainees such as community pediatric providers, pediatric residents, and medical, nursing, and mental health students (with the family’s permission) to observe and learn about developmental coaching. The TREEHOUSE program uses telehealth technology to provide developmental coaching to families. Dedicated interactive developmental coaching provides a window for pediatric providers to positively impact parenting behaviors and reframe expectations early in their child’s life, setting forward a cascade of new possibilities.
Addressing Health Disparities
Health disparities, including racial and ethnic disparities, are a concern nationally with regard to early childhood. There are challenges related to access to health care services: in some states, children who are low-income are 18% less likely to receive EI services, and African American children with developmental delays are 5 times less likely than White children with developmental delays to receive EI services (Marks et al., 2015). Nationally, only 34% of children receive developmental screening and only 7% receive EI services (Keating & Heinemeier, 2022). Disparities related to income are exacerbated by disparities associated with race and ethnicity. Approximately 40% of babies live in poverty nationally, with only 19% of babies in poverty being White (Keating & Heinemeier, 2022). These income, race, and ethnic disparities affect access to care and quality of care. In a study of universal screening for developmental concerns,
children who were White, male, and of higher income were more likely to already be enrolled in early intervention (EI) at the time of
developmental screening... universal develop- mental screening with a validated measure was particularly associated with referral to EI for children who were Black, male, and of lower income. (Wallis et al., 2021, p. 6)
The TREEHOUSE program intentionally targets primary care practitioners and practices who work with low-income and diverse populations to address these health disparities.
The TREEHOUSE Program
The TREEHOUSE program is an adaptation of the Grow Your Kids TREE (Talk Read Engage Encourage) program developed by the MDAAP (Tellerman et al., 2016). The TREE program
has demonstrated acceptability by providers. During an initial feasibility study, 68% of trained pediatric residents at an urban hospital serving primarily Medicaid recipients were highly satisfied or extremely satisfied with the program, and 68% reported the largest barrier to TREE program implementation was time constraints during well–child visits (Rashid & Silver, 2019). The same study found significant increases in the amount providers discussed development and parenting during visits, in documented discussion of parent–child interactions, and in provider confidence in discussing development and parenting. Findings from a completed, quasi-experimental controlled comparison study has also found that parent– child verbal responsivity interactions significantly increased after TREE program implementation for the intervention site compared to the control site (Candelaria et al., 2022). In addition, trained residents reported increases in promoting development and fostering positive interactions and reported increased confidence in conveying child development and providing positive feedback compared to nontrained residents.

There are insufficient infant and early childhood programs and a shortage of properly trained professionals across diverse settings.
The TREEHOUSE program was created during the COVID- 19 pandemic when attending visits in person became more challenging and the need to reach and support families through virtual technology increased. The MDAAP Emotional Health Committee developed the TREEHOUSE program to guide pediatric providers to promote positive parent–child interactions with low-income, Medicaid-enrolled families by performing 30-minute online telehealth video coaching sessions when children are 9 and 15 months old. Its design is timely, with heightened interest in virtual health care delivery options during the COVID-19 response. Its flexibility, innovation, cost and time efficiency, and ease of installation and replicability make it ideal for implementation in busy practices seeking to promote relational health.
The traditional approach to child development in pediatric primary care focuses on surveillance and screening for developmental disabilities. Performing a separate interactive telehealth coaching visit uses development as a vehicle for parents to raise developmental concerns, reflect on the importance of child development, and acquire and practice new skills during the coaching session in talking, reading, and engaging with their young children. These sessions offer an opportunity to foster connections between parents and providers as a relational health concept (Frosch et al., 2019).

Telehealth creates a novel opportunity for the pediatric provider, parents, community visiting nurses or early intervention specialists to meet online simultaneously.
The sessions also create more opportunities to identify needs and connect families with community-based prevention and intervention services. Coaching virtually in the home is a first- line early childhood clinical service intervention and expands the role of pediatric providers to augment and complement the work of statewide EI and other developmental specialists.
In 2021, the Health Resources & Services Administration funded the TREEHOUSE program for 5 years to the University of Maryland School of Social Work (UMB SSW), Institute for Innovation and Implementation (The Institute) and MDAAP. Figure 1 shows the TREEHOUSE program Logic Model including the short-, medium-, and long-term goals. The rest of this article describes the TREEHOUSE program including the intended plan through 2026, outcomes and lessons learned from the first completed cohort, and stories from parents and providers. The broader evaluation seeks to answer the following larger systemic questions. Does the TREEHOUSE program:
1. lead to increased pediatric provider capacity to address patient developmental and social–emotional needs?
2. increase knowledge of and referral to community-based resources to support families?
3. improve the quality of parent–child interactions for low-income families?
4. enhance parent satisfaction with their pediatric providers?
5. strengthen cross-agency partnerships to create an improved system of support for families with young children at the state and local levels?
As the program is in the early stages of project implementation, our discussion will be largely descriptive but includes some preliminary data regarding the first evaluation question.
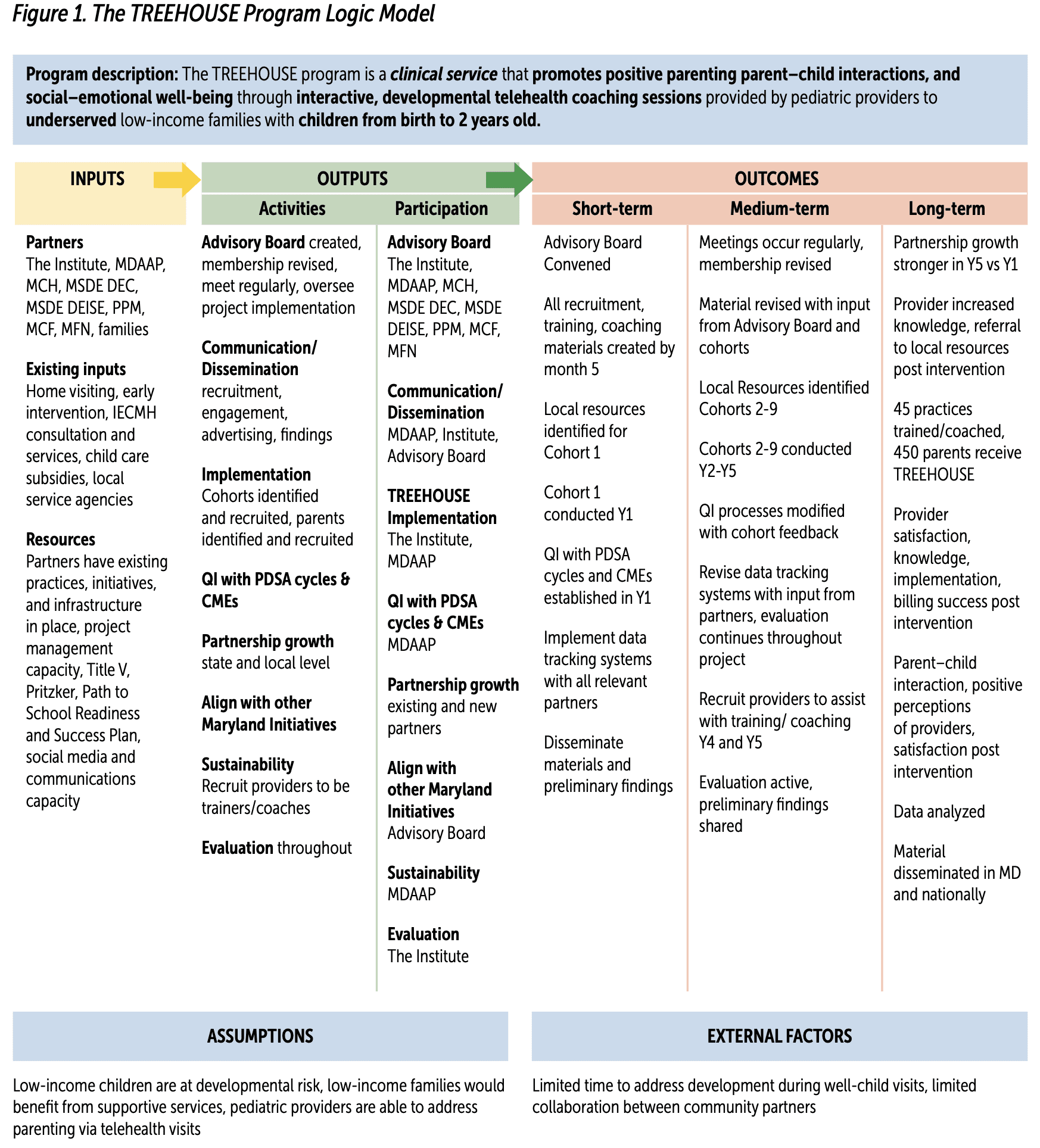
KEY. CME = Continuing Medical Education; IECMH = infant and early childhood mental health; Institute = University of Maryland School of Social Work Institute for Innovation and Implementation; MCF = Maryland Coalition of Families; MCH = MD Department of Maternal Child Health; MDAAP = Maryland Chapter American Academy of Pediatrics; MFN = Maryland Family Network; MSDE DEC = MD State Department of Education Division of Early Childhood; MSDE DEISE = MD State Department of Education Division of Early Intervention and Special Education; PDSA = Plan-Do-Study-Act; PPM = Parents Place of Maryland; QI = Quality Improvement
Target Population
The target population for the TREEHOUSE program are primary care pediatric providers who practice in Maryland. The recruitment goal is to train 9 cohorts of 6–10 pediatric providers over 5 years who practice in a range of settings and locations throughout Maryland to ensure geographic, racial, and socioeconomic diversity in the patient populations. Each pediatric provider is asked to recruit 6–10 parent–child dyads to practice developmental coaching and engage in evaluation data collection. Further, additional providers will be recruited from medical practices that employ previously trained pediatric providers trained in TREEHOUSE to promote sustainability.
Provider Training
The TREEHOUSE Quality Improvement (QI) structure consists of monthly 1-hour meetings occurring for 6 months, conducted by the TREEHOUSE program developers who serve as the co-leaders. These two co-leaders are developmental/behavioral pediatricians with experience in academic institutions and pediatric primary care. Each session consists of a didactic teaching component, provider presentation of their developmental coaching sessions, peer learning through observation of other practitioners, and discussion. Pediatric participants present their patient coaching sessions to the cohort group. A unique component of the training is that by sharing video recordings of their coaching sessions, pediatric providers have an opportunity to observe other practitioners and to provide and receive constructive feedback. The TREEHOUSE co-leaders are also available to provide one-on-one guidance to practitioners as needed. After each QI session, the co-leaders meet with the MDAAP executive director to review the session as a QI/Plan- Do-Study-Act activity.
Parent Coaching Structure
Providers are asked to conduct developmental coaching telehealth appointments when the patient is approximately 9 and/or 15 months old. The 9- and 15-month visits can be for the same child, but families are not required to sign up for two coaching sessions. These developmental appointments, offered outside of well-child visits, are focused on development; parents can raise developmental concerns, as well as acquire and practice new skills in talking, reading, and engaging with young children. Appointments are approximately 30 minutes in length. The coaching sessions are reimbursed by most health insurance carriers including Medicaid.
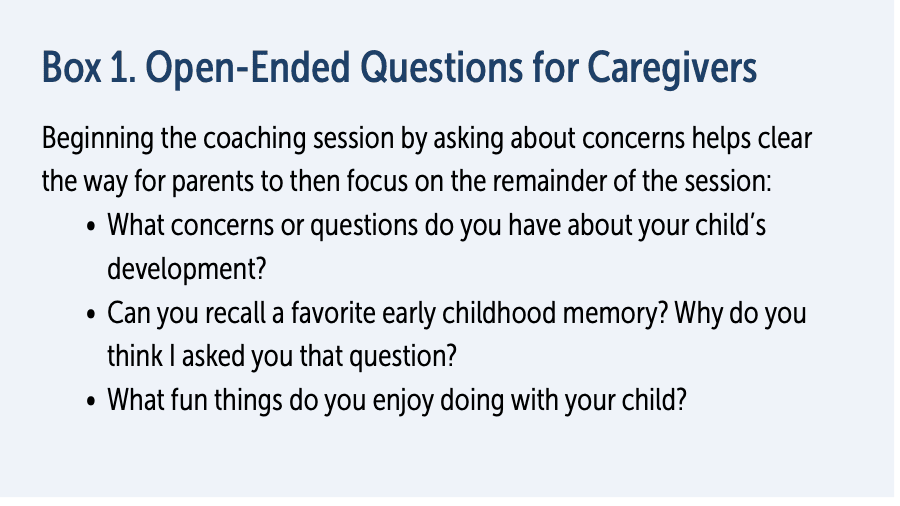
Introduction to the Coaching Session
During coaching sessions, caregivers are engaged in discussion with the pediatric provider through open-ended questions (see Box 1 on p. 60). Asking about early childhood memories helps set the stage for the coaching session. Most caregivers typically relate a memory that involves a relationship with a family member such as a parent, grandparent, or sibling. The memory question helps caregivers extrapolate into the future and consider what types of memories their children will recall in 20–30 years. The question about fun things the caregivers do with the child sets a positive strengths-based tone for the rest of the session in contrast to the deficits-based “what’s wrong?” approach that typifies many health provider–caregiver interactions.
Developmental Domains
Parents are then shown a series of photographs of young children at various stages of development across the domains of communication, motor, cognitive, and social–emotional skills. For example, the motor skills photographs show a series of young children progressing across reaching, sitting, crawling, and standing to point out the head-to-toe nature of motor development. Caregivers are asked to interpret what each set of photographs represents and then estimate “where their child fits in.” A discussion ensues on the next stage of domain development and how caregivers can modify their interactions in concert with their child’s changing skills.
Try It Out
Throughout the coaching sessions, caregivers are encouraged to try out new skills such as the “sports announcer” approach in which parents are guided to narrate what their children are doing as a means of promoting language development. Caregivers are also encouraged to read, play, and sing with their children during the session to highlight the importance of having fun together.
Providing Positive Feedback
Pediatric providers are encouraged to provide caregivers with positive feedback during the sessions to recognize their success and competencies as parents. This type of feedback from a professional can be very powerful particularly when delivered to caregivers who may not be receiving much positive feedback within their personal environment.
What Did You Learn From Today’s Session?
This final component of the session allows caregivers to reflect on what they have taken out of the session, and they are encouraged to continue integrating these new skills into everyday interactions.
The telehealth platform provides a window into the family environment and observes the degree to which families facing limited resources often still provide a stimulating environment with books and toys and create an oasis for their young children. The TREEHOUSE’s developmental coaching model offers a space for families and clinicians to promote relational health. The AAP has called for integrating relational health into pediatric primary care. The TREEHOUSE program provides a template for how this can be accomplished. Subsequent well– child encounters provide opportunities for pediatric providers to reinforce the core components of the program with families.
Additional Program Components
There are several additional components to TREEHOUSE aside from direct provider and parent activities including continuing education, an advisory board, and data collection.
Continuing Education
Pediatric providers enrolled in TREEHOUSE receive continuing education through training and coaching activities. If programmatic and evaluation activities are satisfied, providers can earn 12 CME/Maintenance Of Certification 2 and 25 Maintenance Of Certification 4 credits. Providers complete surveys at baseline and follow up in addition to entering their developmental coaching data into the AAP’s Quality Improvement Data Aggregator (QIDA) system.
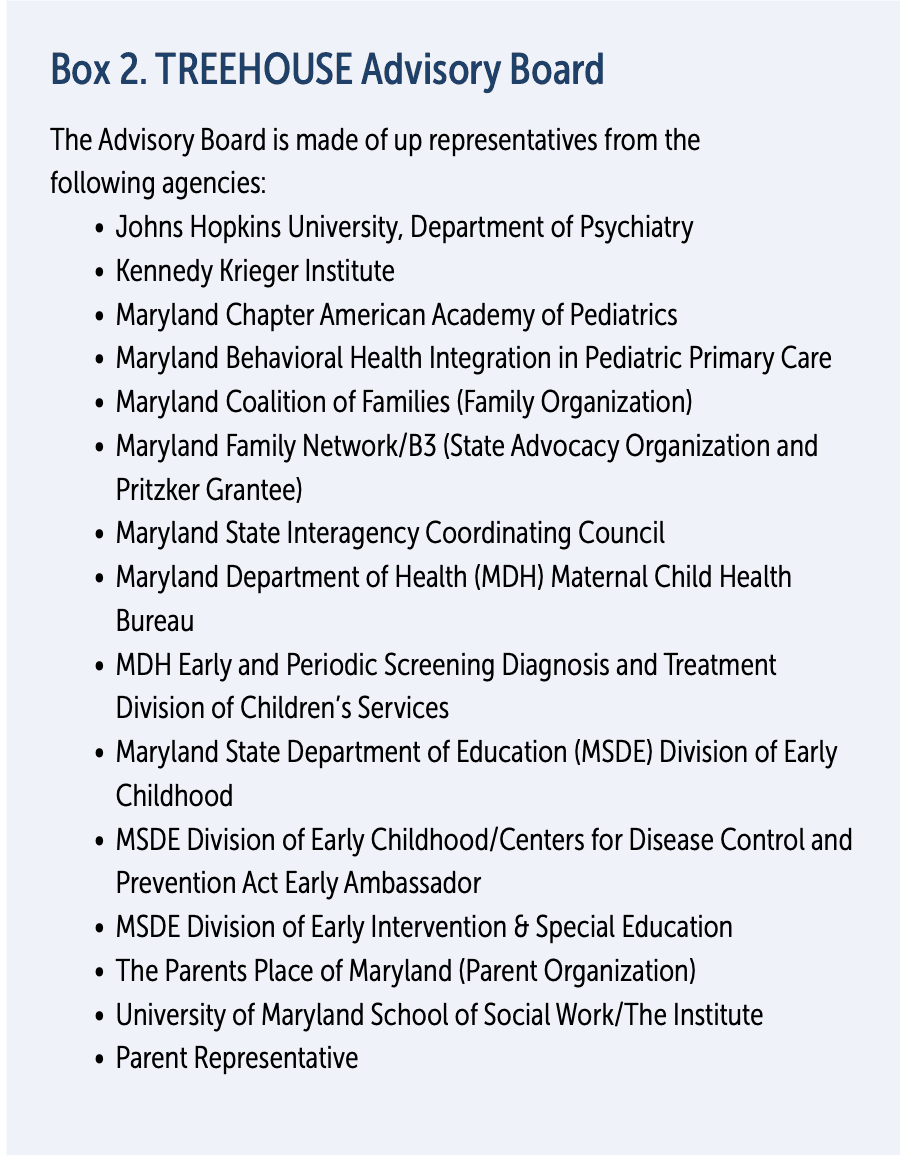
Advisory Board
As a requirement of the funding, there is a statewide TREEHOUSE Advisory Board (see Box 2). The Advisory Board is composed of state and local professionals with expertise in child development and pediatrics. It serves to review the TREEHOUSE QI curriculum for pediatric providers and provide constructive feedback. In addition, they assist with the identification of new providers and sharing effective pediatric provider recruitment strategies. The Advisory Board also helps identify potential future Advisory Board members. Starting in the Fall of 2022 a parent will be added to the Advisory Board to ensure family voice representation. The parent will be compensated for their time. The members of the Advisory Board also complete network analyses, thereby establishing the baseline by which to judge the growth and collaboration levels of the Advisory Board.
Data Collection
Data collection is an integral part of the TREEHOUSE program used to establish whether the program is effective in building clinician skills in the promotion of relational health for providers and in promoting positive parent–child interactions among families.
Provider Measures. The Pediatric Practitioner TREE Questionnaire was previously developed by TREEHOUSE developers and the MDAAP team to assess pediatric perspectives on the importance of promoting positive parent–child interactions and confidence in providing developmental coaching within the TREE program. Electronic medical record data is collected for each cohort to determine TREEHOUSE practices and billing outcomes. After providers have conducted a developmental coaching appointment, they input their coaching data into QIDA. Providers create a separate entry for each patient and report on discussion of developmental topics. These data
are also logged in the pediatric provider’s electronic medical record system.
Process Measures. Meeting notes, attendance records, coaching activities, meeting and training/coaching attendance, and family engagement in coaching sessions are also used to track and refine activities over time. MDAAP monthly feedback QI sessions, internal meetings, and Advisory Board meetings are also used to inform changes over time. Network analysis using the measure (Frey et al., 2006) is administered at all Advisory Board meetings to examine changes in statewide partnership growth over time.
Parent Measures. A demographic questionnaire is administered to collect information about family characteristics (e.g., race, age, socioeconomic status). The StimQ2 (Mendelsohn et al., 2016) is used to measure parent–child reported interactions pre- and post-intervention. The StimQ2 is a structured parent interview/questionnaire that is designed to assess parent–child interactions in the home. The Parents’ Perception of Primary Care (Krugman et al., 2007) is used to measure the relationship and satisfaction with pediatric providers. This is a 22-item parent report questionnaire that assesses the parent’s feelings about how providers behave during visits including perceptions of provider interest in their child’s health, whether the provider spends enough time with them, and whether parents feel comfortable asking questions.
TREEHOUSE Preliminary Outcomes
The TREEHOUSE has begun to examine preliminary findings from the first cohort of providers. A summary is provided in the following sections.
Provider and Practice Information
To date, one cohort of 10 providers has completed the TREEHOUSE program. Nine of the providers have participated in the data collection process. The average age of provider is 55.33 years and the average length of years in practice is 25.44 years. Ninety percent of the cohort was female. One provider identified as Latino, 1 provider identified at Black, 2 identified as Asian, and 6 identified as White. Two providers reported they practiced in urban areas, 7 reported they practice in suburban areas, and 1 reported “other.” The “other” was described as “underserved in any setting.” Three providers reported being in a solo practice, 4 are in a group practice, 2 are hospital-based, and 1 described themselves as a volunteer. Two providers reported having a co-located mental health provider in their practice. Providers served diverse families in Maryland. Seven providers reported their practice served at least 25% Black families, with 4 serving 50% or more Black families. Five providers reported serving between and 10% and 35% Latino families.

Health disparities, including racial and ethnic disparities, are a concern nationally with regard to early childhood.
Providers were asked what screening they conducted in their practices. Eight providers reported using screeners routinely. Three practices reported using one screener, 3 reported using two screeners, and 2 practices reported using three screeners. Six practices reported they use the Reach Out and Read program.
Provider Coaching Sessions
To date, of the 10 providers, 5 have submitted data in QIDA. Of those, there were 30 entries indicating 30 telehealth TREEHOUSE visits were conducted among those 5 providers. Providers have until August 2022 to finalize entry and we expect 2 more providers to enter QIDA data after the time of this publication. There are projected to be an additional 40 entries in QIDA that will reflect a total of 70 visits. Of the 30 current visits, 22 (73.3%) were with families on Medicaid. Three (10%) TREEHOUSE visits led to an outside referral. Thirteen children (43.3%) were 9 months old, 7 (23.3%) were 10 months, and the remaining (n = 10, 32.3%) were between 12 and 18 months. Among the 30 entries, providers reported covering between 60% and 100% of the TREEHOUSE topics. This included 100% for Introductory Content, 63% for Talking and Communication, 67% for Reading, 70% for Motor, 73% for Play and Learning, 87% for Social and Emotional, 100% for Encouragement, and 100% for Parent Feedback.

This final component of the session allows caregivers to reflect on what they have taken out of the session, and they are encouraged to continue integrating these new skills into everyday interactions
Provider Feedback
Of the 5 providers who have completed the QIDA data collection, all of them reported being very or extremely satisfied with the TREEHOUSE program. They also reported that the TREEHOUSE program gave them better insight into the strengths of parents served and 4 reported gaining better insight into challenges faced by parents they served. Four providers reported that they felt parents in their practice have changed their interactions with their children as a result of the TREEHOUSE program. When asked about the benefits of
the TREEHOUSE program, providers made positive comments about their implementation and their interactions with parents. See Box 3 for a full list.
Conclusion
Our data from the TREE program, an intervention delivered during well-child encounters, reveal that the program enhances
caregiver–child interactions and operationalizes the call to promote relational health (Candelaria et al., 2022). Building on that model, the TREEHOUSE program is a brief, inexpensive, easily replicated and learned, universal developmental coaching intervention delivered within a pediatric primary care setting directly by pediatric clinicians. The TREEHOUSE telehealth program is in preliminary phases and has successfully completed one cohort with pediatric providers reporting use of skills and satisfaction with program. We are hopeful that this program will contribute to the deeper ongoing professional conversation on how pediatric providers can actively implement specific practical interventions that promote relational health, resilience, and health equity through capacity and capability building in low-income families and communities.
Learn More
The TREE and TREEHOUSE Programs
www.mdaap.org/tree
Author Bios
Margo Candelaria, PhD, has extensive research and clinical experience with early childhood development and mental health, parent–child interactions, and community systems. Dr. Candelaria has worked with children and parents in medical systems, community mental health agencies, early intervention agencies, Head Start/Early Head Start, school systems, and homelessness and substance use serving agencies. Dr. Candelaria currently serves as the evaluation principal investigator for the Substance Abuse and Mental Health Services Administration (SAMHSA) funded Treatment & Recovery Expansion & Enhancement Project; B’more SUCCEEDS, addressing youth who are substance using and housing unstable with an emphasis on also addressing parenting needs; and the SAMHSA National Child Traumatic Stress Network–funded Family Attachment-focused Services, Treatment, & Training project implementing and evaluating a fast-track, trauma-informed, clinical model addressing early childhood mental health needs. In addition, Dr. Candelaria has served as the evaluation principal investigator for several other the SAMHSA-funded projects focusing on early childhood mental health and parenting supporting such as System of Care, LAUNCH, and Pregnancy Assistance fund grants. Dr. Candelaria has a long history of collaboration with pediatrics including collaboration on telehealth models for the American Academy of Pediatrics (AAP), serving on the Maryland Chapter AAP Emotional Health committee, and collaborating on the TREE project, and is the principal investigator of the Health Resources & Services Administration–funded Healthy Tomorrows project, TREEHOUSE. All of these require tracking of trainings, services, activities, and outcomes across multiple providers and compliance with federally required data collection procedures. Across all these projects, she has focused on program evaluation and implementation science to improve programs for children and families in need by using data and engaging in Continuous Quality Improvement processes.
Ken Tellerman MD, is a general and developmental behavioral pediatrician who has been in private practice in Baltimore
City for more than 35 years. Dr. Tellerman teaches pediatric residents from Johns Hopkins, University of Maryland, and Sinai Medical Centers during their behavioral health rotations. As chair of the Maryland Chapter American Academy of Pediatrics Emotional Health Committee for more than 25 years, he has been involved in multiple teaching programs throughout Maryland, training practitioners in developmental and behavioral pediatrics. He is one of the chief developers of the Grow Your Kids: TREE and TREEHOUSE programs that train pediatric practitioners to perform developmental coaching during office- based well-child encounters and through telehealth sessions. He is also one of the medical directors for the nonprofit OCHO (Organization for Community Health Outreach) which provides health care in Honduras.
Anna Maria Wilms Floet, MD, FAAP, is a developmental behavioral pediatrician. Dr. Wilms Floet has been in practice for 25 years and specializes in the evaluation of young children with suspected autism spectrum disorder. She is an assistant professor of pediatrics at Johns Hopkins University. Dr. Wilms Floet serves on the Maryland State Interagency Coordinating Council (0–5). She serves as rotation lead for pediatric trainees in their developmental/behavioral rotation and participates in teaching activities at Kennedy Krieger Institute. Dr. Wilms Floet is one of the co-developers of TREEHOUSE program.
Heather Whitty, MA, supports the evaluation unit of the Parent Infant Early Childhood team at the Institute for Innovation
and Implementation through data analysis and research staff supervision. Current projects in which she chiefly manages the data include two Substance Abuse and Mental Health Services Administration grants (an Early Childhood Systems of Care grant, ESMART, a National Child Traumatic Stress Initiative grant, FASTT) and two Health and Human Services grants (PACE IT and TREEHOUSE). Ms. Whitty provides individuals and groups with technical assistance in entering data, develops protocols related to data cleaning and management, analyses the data, and reports on outcomes via program and state-level reports. Former projects at The Institute include another Early Childhood System of Care grant, BRIDGE, the Teaching, Reading, Engaging, Encouraging (TREE) project, and the Howard County Individualized Family Service Plan Evaluation. Ms. Whitty comes to this work with 16 years of experience in early childhood development, education, and research. She has worked within hospital and post-secondary research institutes in the USA and in Canada. Ms. Whitty previously managed a large, mixed methods study investigating mental health and health service utilization of adolescent mothers at The Offord Center for Child Studies at McMaster University.
Suggested Citaiton
Candelaria, M., Tellerman, K., Wilms Floet, A. M., & Whitty, H. (2022). The TREEHOUSE Program: Promoting early childhood development and parent–child interaction via telehealth in pediatrics. ZERO TO THREE Journal, 43(1), 55–65.
References
American Board of Pediatrics. (2018, May 8). Behavioral and mental health: Gaps and challenges. The American Board of Pediatrics. www.abp.org/news/behavioral-and-mental-health-gaps-and-challenges
Brockmeyer-Cates, C., Weisleder, A., & Mendelsohn, A. (2016). Mitigating the effects of family poverty on early child development through parenting interventions in primary care. Academic Pediatrics, 16(3), S112–S120. https://doi.org/10.1016/j.acap.2015.12.015. www.academicpedsjnl.net/article/S1876-2859(15)00388-5/fulltext
Bucci, M., Marques, S. S., Oh, D., & Harris, N. B. (2016). Toxic stress in children and adolescents. Advances in Pediatrics, 63(1), 403–428. https://doi.org/10.1016/j.yapd.2016.04.002. www.advancesinpediatrics.com/article/S0065-3101(16)30002-0/fulltext
Candelaria, M. (University of Maryland School of Social Work), Tellerman, K., Whitty, H., Silver, D., Feigelman, S., Endy, K., Afkinich, J., & Wilms Floet, A. (2022). The TREE program: Promoting positive parent-child interactions during well child visits [Manuscript submitted for publication].
Center on the Developing Child. (2016). From best practices to breakthrough impacts: A science-based approach to building a more promising future for young children and families. Harvard University. https://developingchild.harvard.edu/resources/from-best-practices-to-breakthrough-impacts
Center on the Developing Child. (2019). A guide to toxic stress. https://developingchild.harvard.edu/guide/a-guide-to-toxic-stress
Felitti, V. J., Anda, R. F., Nordenberg, D., Williamson, D. F., Spitz, A. M., Edwards, V., Koss, M. P., & Marks, J. S. (1998). Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults. American Journal of Preventive Medicine, 14(4), 245–258. www.ajpmonline.org/article/S0749-3797(98)00017-8/fulltext
Fierman, A. H., Beck, A. F., Chung, E. K., Tschudy, M. M., Coker, T. R., Mistry, K. B., Siegel, B., Chamberlain, L. J., Conroy, K., Federico, S. G., Flanagan, P. J., Garg, A., Gitterman, B. A., Grace, A. M., Gross, R. S., Hole, M. K., Klass, P., Kraft, C., Kuo, A., ... Cox, J. (2016). Redesigning health care practices to address childhood poverty. Academic Pediatrics, 16(3), S136–S146. https://doi.org/10.1016/j.acap.2016.01.004. www.academicpedsjnl.net/article/S1876-2859(16)00020-6/fulltext
Folger, A. T., Eismann, E. A., Stephenson, N. B., Shapiro, R. A., Macaluso, M., Brownrigg, M. E., & Gillespie, R. J. (2018). Parental adverse childhood experiences and offspring development at 2 years of age. Pediatrics, 141(4), e20172826. https://doi.org/10.1542/peds.2017-2826. https://publications.aap.org/pediatrics/article/141/4/e20172826/37806/Parental-Adverse-Childhood-Experiences-and
Freed, G. L., Dunham, K. M., Switalski, K. E., Jones, M. D., & McGuinness, G. A. (2009). Recently trained general pediatricians: Perspectives on residency training and scope of practice. Pediatrics, 123(Supp. 1), S38– S43. https://doi.org/10.1542/peds.2008-1578J. https://publications. aap.org/pediatrics/article-abstract/123/Supplement_1/S38/29623/Recently-Trained-General-Pediatricians?redirectedFrom=fulltext
Frey, B., Lohmeier, J., Lee, S. W., & Tollefson, N. (2006). Measuring collaboration among grant partners. https://doi.org/10.1177/1098214006290356. https://journals.sagepub.com/doi/10.1177/1098214006290356
Frosch, C. A., Schoppe-Sullivan, S. J., & O’Banion, D. D. (2019). Parenting and child development: A relational health perspective. American Journal of Lifestyle Medicine, 15(1), 45–59. https://doi.org/10.1177/1559827619849028. https://journals.sagepub.com/doi/10.1177/1559827619849028
Garner, A., Yogman, M., & Section on Developmental and Behavioral Pediatrics, Council on Early Childhood Committee on Psychosocial Aspects of Child and Family Health. (2021). Preventing childhood toxic stress: Partnering with families and communities to promote relational health. Pediatrics, 148(2). https://doi.org/10.1542/peds.2021-052582. https://publications.aap.org/pediatrics/article/148/2/e2021052582/179805/Preventing-Childhood-Toxic-Stress-Partnering-With
Garner, P. W., & Waajid, B. (2012). Emotion knowledge and self-regulation as predictors of preschoolers’ cognitive ability, classroom behavior, and social competence. Journal of Psychoeducational Assessment, 30(4), 330–343. https://doi.org/10.1177/0734282912449441. https://journals.sagepub.com/doi/10.1177/0734282912449441
Ginsburg, K. R., the Committee on Communications, & the Committee on Psychosocial Aspects of Child and Family Health. (2007). The importance of play in promoting healthy child development and maintaining strong parent-child bonds. Pediatrics, 119(1), 182–191. https://doi.org/10.1542/peds.2006-2697. https://publications.aap.org/pediatrics/article/119/1/182/70699/The-Importance-of-Play-in-Promoting-Healthy-Child
Gross, D., Garvey, C., Julion, W., Fogg, L., Tucker, S., & Mokros, H. (2009). Efficacy of the Chicago Parent Program with low-income African American and Latino parents of young children. Prevention Science, 10(1), 54–65. https://doi.org/10.1007/s11121-008-0116-7. https://link.springer.com/article/10.1007/s11121-008-0116-7
Hagan, F. J., Shaw, J. S., & Duncan, P. M. (2017). Bright Futures: Guidelines for health supervision of infants, children and adolescents (4th ed.). American Academy of Pediatrics.
Hart, B., & Risley, T. R. (1995). Meaningful differences in the everyday experience of young American children. Brookes.
Hebbeler, K., Spiker, D., Bailey, D., Scarborough, A., Mallik, S., Simeonsson, R., Singer, M., & Nelson, L. (2007). Early intervention for infants and toddlers with disabilities and their families: Participants, services, and outcomes (National Early Intervention Longitudinal Study [NEILS]). Stanford Research Institute International. https://www.sri.com/wp-content/uploads/2021/12/neils_finalreport_200702.pdf
High, P. C. (2014). Literacy promotion: An essential component of primary care pediatric practice. Pediatrics, 134(2), 404–409. https://doi.org/10.1542/peds.2014-1384
Horwitz, S. M., Hurlburt, M. S., Heneghan, A., Zhang, J., Rolls-Reutz, J., Fisher, E., Landsverk, J., & Stein, R. E. K. (2012). Mental health problems in young children investigated by U.S. child welfare agencies. Journal of the American Academy of Child & Adolescent Psychiatry, 51(6), 572–581. https://doi.org/10.1016/j.jaac.2012.03.006. https://www.jaacap.org/article/S0890-8567(12)00227-4/fulltext
Jimenez, M. E., Fiks, A. G., Shah, L. R., Gerdes, M., Ni, A. Y., Pati, S., & Guevara, J. P. (2014). Factors associated with early intervention referral and evaluation: A mixed methods analysis. Academic Pediatrics, 14(3), 315–323. https://doi.org/10.1016/j.acap.2014.01.007. www.academicpedsjnl.net/article/S1876-2859(14)00009-6/fulltext
Johnson, S. B., Riley, A. W., Granger, D. A., & Riis, J. (2013). The science of early life toxic stress for pediatric practice and advocacy. Pediatrics, 131(2), 319–327. https://doi.org/10.1542/peds.2012-0469. https://publications.aap.org/pediatrics/article-abstract/131/2/319/31871/ The-Science-of-Early-Life-Toxic-Stress-for?redirectedFrom=fulltext
Keating, K., & Heinemeier, S. (2022). State of babies yearbook 2022. ZERO TO THREE. https://stateofbabies.org
Krugman, S. D., Racine, A., Dabrow, S., Sanguino, S., Meyer, W., Seid, M., & Serwint, J. R. (2007). Measuring primary care of children in pediatric resident continuity practices: A Continuity Research Network study. Pediatrics, 120(2), e262–e271. https://doi.org/10.1542/peds.2006-1346. https://publications.aap.org/pediatrics/article-abstract/120/2/e262/70436/Measuring-Primary-Care-of-Children-in-Pediatric?redirectedFrom=fulltext
Leffel, K., & Suskind, D. (2013). Parent-directed approaches to enrich the early language environments of children living in poverty. Seminars in Speech and Language, 34(04), 267–278. https://doi.org/10.1055/s-0033-1353443. www.thieme-connect.de/products/ejournals/abstract/10.1055/s-0033-1353443
Lillard, A., Lerner, M., Hopkins, E. J., Dore, R. A., Smith, E. D., & Palmquist, C. (2013). The impact of pretend play on children’s development: A review of the evidence. https://doi.apa.org/doiLanding?doi=10.1037/a0029321. https://psycnet.apa.org/doiLanding?doi=10.1037%2Fa0029321
Lipkin, P., Macias, M., Baer Chen, B., Coury, D., Gottschlich, E. A., Hyman, S. L., Sisk, B., Wolfe, A., & Levy, S. E. (2020). Trends in pediatricians’ developmental screening: 2002–2016. Pediatrics, 145(4), e20190851. https://doi.org/10.1542/peds.2019-0851. https://publications.aap.org/pediatrics/article/145/4/e20190851/76927/Trends-in-Pediatricians-Developmental-Screening
Marks, K. P., Griffen, A. K., Herrera, P., Macias, M. M., Rice, C. E., & Robinson, C. (2015). Systemwide solutions to improve early intervention for developmental- behavioral concerns. Pediatrics, 136(6), e1492–e1494. https://doi.org/10.1542/peds.2015-1723. https://publications.aap.org/pediatrics/article-abstract/136/6/e1492/33873/Systemwide-Solutions-to-Improve-Early-Intervention?redirectedFrom=fulltext
Mendelsohn, A. L., Cates, C. B., Johnson, M., Weisleder, A., & Dryer, B. (2016). STIMQ2. New York University School of Medicine.
Milteer, R. M., Ginsburg, K. R., Council on Communications and Media Committee on Psychosocial Aspects of Child and Family Health, & Mulligan, D. A. (2012). The importance of play in promoting healthy child development and maintaining strong parent-child bond: Focus on children in poverty. Pediatrics, 129(1), e204–e213. https://doi.org/10.1542/peds.2011-2953. https://publications.aap.org/pediatrics/article/129/1/e204/31545/The-Importance-of-Play-in-Promoting-Healthy-Child
National Research Council & Institute of Medicine. (2000). From neurons to neighborhoods: The science of early childhood development. J. P. Shonkoff & D. A. Phillips, (Eds.), Board on Children, Youth, and Families; Commission on Behavioral and Social Sciences and Education. National Academy Press.
Needlman, R., Toker, K. H., Dreyer, B. P., Klass, P., & Mendelsohn, A. L. (2005). Effectiveness of a primary care intervention to support reading aloud: A multicenter evaluation. Ambulatory Pediatrics, 5(4), 209–215. https://doi.org/10.1367/A04-110R.1. www.sciencedirect.com/science/article/abs/pii/S1530156705602043?via%3Dihub
Nelson, B., Dudovitz, R., Coker, T., Barnert, E., Biely, C., Li, N., Szilagyi, P., Larson, K., Halfon, N., Zimmerman, F., & Chung, P. (2016). Predictors of poor school readiness in children without developmental delay at age 2. Pediatrics, 138(2), e 20154477.
Olson, C. A., McSwain, S. D., Curfman, A. L., & Chuo, J. (2018). The current pediatric telehealth landscape. Pediatrics, 141(3), e20172334. https://doi.org/10.1542/peds.2017-2334. https://publications.aap.org/pediatrics/article/141/3/e20172334/37605/The-Current-Pediatric-Telehealth-Landscape
Rashid, H., & Silver, D. (2019, April). Bringing “Grow Your Kids: TREE” a positive parenting tool to a busy, teaching clinic: A feasibility study [Conference session]. Pediatric Academic Societies Meeting, Baltimore, MD.
Rush, D. D., & Shelden, M. L. (2020). The early childhood coaching handbook (2nd ed.). Brookes.
Shah, P., Kaciroti, N., Richards, B., Oh, W., & Lumeng, J. C. (2016). Developmental outcomes of late preterm infants from infancy to kindergarten. Pediatrics, 138(2), e20153496. https://doi.org/10.1542/peds.2015-3496. https://publications.aap.org/pediatrics/article-abstract/138/2/e20153496/52425/Developmental-Outcomes-of-Late-Preterm-Infants?redirectedFrom=fulltext
Shah, R., Sobotka, S. A., Chen, Y.-F., & Msall, M. E. (2015). Positive parenting practices, health disparities, and developmental progress. Pediatrics, 136(2), 318–326. https://doi.org/10.1542/peds.2014-3390. https://publications.aap.org/pediatrics/article-abstract/136/2/318/33787/ Positive-Parenting-Practices-Health-Disparities?redirectedFrom=fulltext
Sheely-Moore, A. I., & Bratton, S. C. (2010). A strengths-based parenting intervention with low-income African American families. Professional School Counseling, 13(3), 2156759X1001300. https://doi. org/10.1177/2156759X1001300305. https://journals.sagepub.com/doi/10.1177/2156759X1001300305
Shonkoff, J. P. (2014). Changing the narrative for early childhood investment. JAMA Pediatrics, 168(2), 105. https://doi.org/10.1001/jamapediatrics.2013.4212. https://jamanetwork.com/journals/jamapediatrics/article-abstract/1785479
Shonkoff, J. P., Garner, A. S., The Committee on Psychosocial Aspects of Child and Family Health, Committee on Early Childhood, Siegel, B. S., Dobbins, M. I., Earls, M. F., Garner, A. S., McGuinn, L., Pascoe, J., & Wood, D. L. (2012). The lifelong effects of early childhood adversity and toxic stress. Pediatrics, 129(1), e232–e246. https://doi.org/10.1542/peds.2011-2663. https://publications.aap.org/pediatrics/article/129/1/e232/31628/The-Lifelong-Effects-of-Early-Childhood-Adversity
Tamis-LeMonda, C. S., Bornstein, M. H., & Baumwell, L. (2001). Maternal responsiveness and children’s achievement of language milestones. Child Development, 72(3), 748–767. https://doi.org/10.1111/1467-8624.00313. https://srcd.onlinelibrary.wiley.com/doi/10.1111/1467-8624.00313
Tamis-LeMonda, C. S., Shannon, J. D., Cabrera, N. J., & Lamb, M. E. (2004). Fathers and mothers at play with their 2- and 3-year-olds: Contributions to language and cognitive development. Child Development, 75(6), 1806–1820. https://doi.org/10.1111/j.1467-8624.2004.00818.x. https://srcd. onlinelibrary.wiley.com/doi/10.1111/j.1467-8624.2004.00818.x
Tellerman, K., Candelaria, M., Chaikind, L., Harrison, J., Howard, B., Spicyn, N., & Wilms-Floet, A. (2016). GROW YOUR KIDS: TREE (Talk Read Engage Encourage) office manual for pediatric practitioners. Maryland Chapter Academy of Pediatrics. www.mdaap.org/pdf/GROW%20YOUR%20KIDS%20TREE%20MANUAL%20April.pdf
Traub, F., & Boynton-Jarrett, R. (2017). Modifiable resilience factors to childhood adversity for clinical pediatric practice. Pediatrics, 139(5), e20162569. https://doi.org/10.1542/peds.2016-2569. https://publications.aap.org/pediatrics/article-abstract/139/5/e20162569/38752/Modifiable-Resilience-Factors-to-Childhood?redirectedFrom=fulltext
Wallis, K. E., Davis Rivera, L. B., Guthrie, W., Bennett, A. E., Mandell, D. S., & Miller, J. S. (2021). Provider responses to positive developmental screening: Disparities in referral practices? Journal of Developmental & Behavioral Pediatrics, 42(1), 23–31. https://doi.org/10.1097/DBP.0000000000000855. https://journals.lww.com/jrnldbp/Abstract/2021/01000/Provider_Responses_to_Positive_Developmental.4.aspx
Weisleder, A., Cates, C. B., Dreyer, B. P., Johnson, S. B., Huberman, H. S., Seery, A. M., Canfield, C. F., & Mendelsohn, A. L. (2016). Promotion of positive parenting and prevention of socioemotional disparities. Pediatrics, 137(2). https://doi.org/10.1542/peds.2015-3239. https://publications.aap.org/pediatrics/article-abstract/137/2/e20153239/52737/Promotion-of-Positive-Parenting-and-Prevention-of?redirectedFrom=fulltext
Williams, R. C., Biscaro, A., & Clinton, J. (2019). Relationships matter: How clinicians can support positive parenting in the early years. Paediatrics & Child Health, 24(5), 340–347. https://doi.org/10.1093/pch/pxz063. https://academic.oup.com/pch/article/24/5/340/5538271
Yogman, M., Garner, A., Hutchinson, J., Hirsh-Pasek, K., Golinkoff, R. M., Committee on Psychosocial Aspects of Child and Family Health, & Council on Communications and Media. (2018). The power of play: A pediatric role in enhancing development in young children. Pediatrics, 142(3), e20182058. https://doi.org/10.1542/peds.2018-2058. https://publications.aap.org/pediatrics/article/142/3/e20182058/38649/The-Power-of-Play-A-Pediatric-Role-in-Enhancing
ZERO TO THREE. (2018). Millennial connections. National Parent Survey: Millennial Connections. www.zerotothree.org/resources/series/national-parent-survey-millennial-connections#explore-key-findings